Celebrating '20 Years of Discovery' at ASU Biodesign Institute

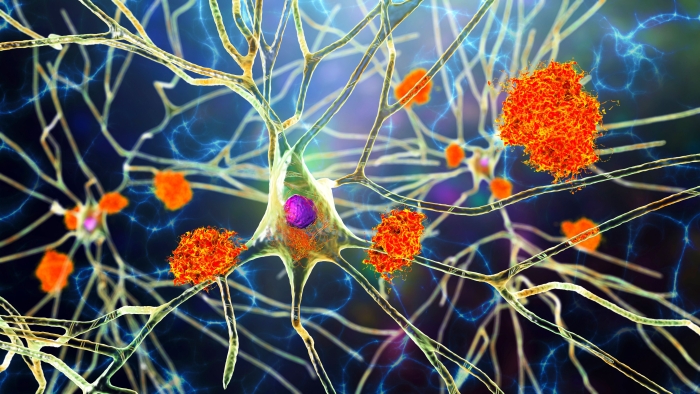
Graphic by Jason Drees/ASU
Editor’s note: The Biodesign Institute at Arizona State University is celebrating its landmark 20th anniversary. This is the first installment in a series called “20 Years of Discovery.” Each story reflects on several groundbreaking scientific discoveries and impactful innovations made since the institute was opened in 2004.
The Biodesign Institute at Arizona State University, pioneered by visionary plant biologist Charles Arntzen, is an incubator for scientific breakthroughs — pushing the boundaries of what's possible in nature-inspired research and the frontiers of bioscience. These innovations have reshaped our understanding of life and its workings and led to practical applications that have improved life on Earth.
Here, we revisit several impactful and ingenious discoveries from a vast portfolio of research that embodies the institute's commitment to creating a healthier and more sustainable future for all.
Innovating to support Arizona during the COVID-19 pandemic
In 2019, SARS-CoV-2, a deadly viral contagion, took root in the United States. In less than two years, the novel virus claimed more than one million lives in the U.S. and close to 7 million globally, as scientists around the world engaged in a frenzied race against the disease.
Amid the chaos, the Biodesign Institute emerged as a leader in the state’s response to the pandemic.
Led by Executive Director Dr. Joshua LaBaer, a team at the Biodesign Institute developed Arizona’s first easy-to-use saliva-based COVID-19 diagnostic test in 2020.
This revolutionary diagnostic tool increased accessibility to COVID-19 testing and offered test results typically in less than 48 hours. This helped provide invaluable public health information to state leaders and hospitals on the prevalence and spread of the disease.
The test detects the virus through saliva samples that people collect themselves.
“We realized that testing was the key to understanding where this deadly virus was going,” LaBaer says. “Every decision we made was based on how to save the greatest number of people, identify the largest number of cases and get the answer out there.”
ASU received FDA emergency authorization for the test and quickly transitioned its COVID-19 testing from nasopharyngeal to saliva-based analysis. The Biodesign Institute rapidly mobilized and leveraged the innovative saliva-based test, reaching a milestone of 1 million COVID-19 tests in Arizona by October 2021.
Next, Biodesign researchers began to unravel the mysteries of the virus' multiple variants, launching aggressive efforts to understand SARS-CoV-2 transmission and evolution by using advanced genomic sequencing and functional studies of mutations. The institute’s exceptional ability to both test and sequence the virus, all under one roof, supported time-sensitive tracking of the pandemic.
Biodesign researchers identified and sequenced the first COVID-19 cases in Arizona and discovered a state variant called B.1.243.1 carrying the E484K, or "eek," mutation. Biodesign, in collaboration with state health authorities, tracked the spread of variants across Arizona.
Today, researchers at the institute continue to investigate how new variants evade the immune system, trace the ancestry and worldwide movement of the virus by analyzing its genetic code, explore where the virus may be spreading in animal populations, and evaluate whether the pathogen's high mutation rate could also be its Achilles' heel — all crucial efforts in the ongoing fight against COVID-19.
Ever on the lookout for new techniques to detect disease, the institute also harnessed the power of wastewater-based epidemiology, discovering the presence of SARS-CoV-2 in community sewage systems. This unique approach became instrumental in forecasting outbreaks and shaping public health policies, particularly in the city of Tempe.
Wastewater surveillance, described as “an information superhighway under your feet,” is an emerging tool for early detection of disease outbreaks like influenza, COVID-19 and opioids.
A new generation of vaccines targets multiple diseases
For years, the Biodesign Institute has been at the forefront of developing innovative vaccines by using unconventional platforms. One significant breakthrough involved creating the world’s first plant-based Zika vaccine in 2017.
The new approach involves producing a vaccine derived from tobacco plants, making them potentially more potent, and safer and cheaper to produce than any other efforts to date.
The use of less costly vaccine alternatives would be enormously beneficial, particularly in the developing world. This would help address both economic and health challenges associated with Zika — a viral pathogen responsible for serious birth abnormalities.
The institute’s pioneering work also includes therapeutics to address Ebola — one of the planet’s deadliest pathogens. The roots of the world’s first cure for Ebola can be traced to the institute in 2001, where Biodesign founder Charles Arntzen’s research laid the foundation.
Using another tobacco-based platform, Arntzen, in collaboration with San Diego-based MAPP Biopharmaceutical and Kentucky Bioprocessing, engineered a powerful monoclonal antibody cocktail.
The treatment was used to save the lives of two missionaries stricken with the illness at the height of the West African Ebola outbreak. Both made a full recovery. This was a major win for the institute — saving lives and garnering a flood of media and scientific attention from around the world.
“The newswires were alive with stories with titles such as ‘Secret serum likely saved Ebola patients,’” Arntzen recalls. “It was hardly a secret to (ZMapp founder) Larry Zeitlin and me, or our colleagues, who had been working for over a decade on finding a lifesaving Ebola therapeutic.”
Using another platform, the Biodesign Center forInfectious Disease and Vaccinology developed a suite of powerful vaccines using bioengineered Salmonella viruses that act as vaccine carriers. Scientists developed a self-destructing Salmonella vaccine delivery system designed to enable efficient colonization by the bacterium and stimulate an immune response upon the rupture of bacterial cells.
The self-destructing mechanism of Salmonella makes it a promising platform for delivering oral DNA vaccines, with the benefit of very low manufacturing costs. This approach is being explored for a variety of illnesses, including bacterial pneumonia, influenza, and other infectious diseases in both humans and agricultural animals.
In addition to developing new vaccines to combat infectious diseases, researchers are working to harness the body’s immune system to combat drug addiction.
One such approach is a vaccine to fight nicotine dependence. The vaccine uses tiny particles affixed to a scaffold constructed from DNA. The nanodevice can train the immune system to recruit antibodies to bind with nicotine, reducing nicotine cravings and making it easier for people to quit smoking. A successful vaccine could help reduce one of the predominant sources of preventable death.
Another exciting area of research involves the quest for an anti-cancer vaccine. Unlike traditional approaches, which target personal mutations unique to each individual's cancer, this innovative vaccine focuses on shared mutations present in most individuals with a specific cancer subtype.
The vaccine's effectiveness was demonstrated in a mouse model of breast cancer, where it showed significant promise in eradicating the disease.
The researchers are also testing a shared vaccine as a preventive measure in a clinical trial of cancer in dogs. The shared vaccine strategy is also being explored for the treatment of other cancers, including pediatric brain cancer.
New insights in neuroscience
The Biodesign ASU-Banner Neurodegenerative Disease Research Center is advancing our knowledge of neurodegenerative diseases, providing new insights into the mechanisms behind these conditions and offering hope for future treatments.
"The NDRC’s main mission is to reverse disability and suffering of individuals with neurodegenerative diseases, and also diminish the burden of their caregivers," says Jeffrey Kordower, director of the center and professor in ASU's School of Life Sciences.
Choline, an essential nutrient found in various foods, is critical for bodily functions, including brain health. Research at the Biodesign Institute has explored the impact of dietary choline deficiency on systemic health and its potential link to neurodegenerative diseases such as Alzheimer's.
Scientists have discovered that not having enough choline can change the way groups of nerve cells work in the brain's hippocampus. This affects scaffolded structures within cells and how cells communicate with each other at their connecting points. These functions are essential for the brain to work properly.
Disruptions in choline levels have been linked to altered protein networks related to insulin metabolism, mitochondrial function, inflammation and metabolic processing. Significantly, choline is necessary to produce acetylcholine, a neurotransmitter pivotal for memory and muscle control. Despite its importance, studies suggest that most people do not receive the recommended amount of choline, which may exacerbate the progression of Alzheimer's disease.
A groundbreaking study by ASU in 2018, in collaboration with other institutions, has indicated a potential viral connection to Alzheimer's disease.
The research, using post-mortem brain samples, points to species of herpesvirus as contributors to the disorder's development. This novel perspective on the pathogenesis of Alzheimer's disease could lead to new approaches in understanding and treating the disease.
Working together, the ASU-Banner Neurodegenerative Disease Research Center and the Biodesign Center for Bioenergetics have significantly advanced our understanding of Alzheimer's disease, particularly concerning mitochondrial function.
Mitochondria, vital for cell energy production, have been identified as central in the progressive, degenerative pathology of Alzheimer’s. Researchers found that molecular signals sent by the mitochondria to the cell nucleus, which help produce vital proteins, can become altered even decades before the onset of clinical symptoms of the disease.
Recognizing these cellular signals could help identify changes linked with Alzheimer’s and other neurodegenerative diseases in their earliest stages.
Other efforts include the development of small molecule drugs in 2019, called kinase inhibitors, which show promise for early intervention in the brain’s production of plaques and tangles, two classic hallmarks of Alzheimer’s disease. Overall, this research marks a pivotal step in understanding the molecular and genetic basis of Alzheimer's and opens new possibilities for early detection and treatment strategies.
The institute has also made significant strides in the study of Parkinson's disease, including research on engineering neuronal cells to replace or repair the damaged neural circuits in people with the disease. This approach can potentially restore function in the affected areas of the brain, offering an exciting new avenue for treatment.
'20 Years of Discovery' at ASU's Biodesign Institute
Explore the other installments in this series:
More Science and technology

Breakthrough copper alloy achieves unprecedented high-temperature performance
A team of researchers from Arizona State University, the U.S. Army Research Laboratory, Lehigh University and Louisiana State University has developed a groundbreaking high-temperature copper alloy…

4 ASU researchers named senior members of the National Academy of Inventors
The National Academy of Inventors recently named four Arizona State University researchers as senior members to the prestigious organization.Professor Qiang Chen and associate professors Matthew…

Transforming Arizona’s highways for a smoother drive
Imagine you’re driving down a smooth stretch of road. Your tires have firm traction. There are no potholes you need to swerve to avoid. Your suspension feels responsive. You’re relaxed and focused on…