'20 Years of Discovery' at ASU's Biodesign Institute: Diagnostics, DNA research and plant-based therapies

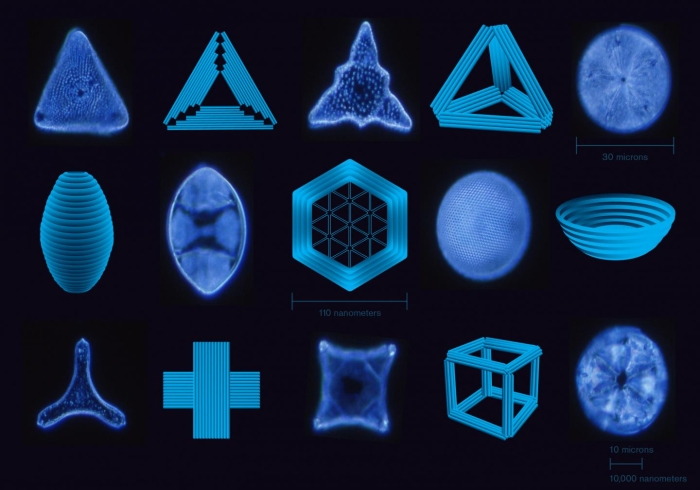
Graphic by Jason Drees/ASU
Editor’s note: The Biodesign Institute at Arizona State University is celebrating its landmark 20th anniversary. This is the fourth installment in a series called “20 Years of Discovery.” Each story reflects on groundbreaking scientific discoveries and impactful innovations made since the institute was founded in 2004.
The Biodesign Institute at Arizona State University works on multiple fronts to advance medical knowledge, develop life-saving therapies and improve well-being for people around the world.
This segment highlights the development of innovative tools for rapid, accurate and low-cost medical diagnoses, many suited for use in the developing world; using DNA — the molecule of life — as a building material to spur the development of new nanotechnologies; and, finally, innovative ways to use plants to produce powerful treatments and vaccines that target multiple infectious diseases.
Transforming health: Biodesign’s diagnostic revolution
African Swine Fever (ASF) is a highly contagious and often lethal disease that has devastated swine populations globally. Traditional diagnostic methods are costly and time-consuming, hindering the swift containment of outbreaks.
Biodesign researchers have introduced a novel method called NaSRED (nanoparticle-supported rapid electronic detection). This technique significantly reduces the time and cost of diagnosing the disease, providing results in minutes and offering superior sensitivity compared with current standards. NaSRED’s ability to detect ASF in the field without sophisticated laboratory equipment promises to revolutionize disease management and protect swine populations worldwide.
NaSRED’s diagnostic sensitivity is estimated to be more than 10 times greater than that of enzyme-linked immunosorbent assays — currently considered the gold standard for such tests. This basic technique has already demonstrated impressive results, as an earlier prototype successfully identified the presence of two global human pathogens: SARS-CoV-2 and Ebola.
“The structure of the ASF virus is exceptionally complex, compared with more familiar viruses, including SARS-CoV-2,” according to Chao Wang, lead author of the study. “This has made vaccine development far more challenging than for other viral pathogens. A rapid, cost-effective diagnostic method like the one we are developing remains our best tool against this pervasive threat.”
Another vexing health challenge is valley fever — caused by inhaling spores of the fungus coccidioides — particularly in the arid regions of the American Southwest. Traditional diagnostic methods have a high false negative rate, making accurate detection difficult.
Biodesign researchers with the Center for Innovations in Medicine have developed a far-reaching diagnostic technique called immunosignaturing. This method uses a microarray platform to create a detailed profile of immune activity from a small blood sample, typically less than a microliter. Immunosignaturing has demonstrated a remarkable 98% accuracy in distinguishing valley fever from other infections and can identify false negatives with 100% accuracy.
This advancement offers a promising tool for accurate, cost-effective and rapid diagnosis, potentially improving patient outcomes and disease management.
Biodesign researchers are investigating how evolution enables the adaptation of living forms to environmental challenges, through which chance mutations and selective pressures allow some species to thrive while others face extinction.
Scientists have explored how these evolutionary processes can be subverted, resulting in cancer. Their research focuses on Barrett’s esophagus, a condition affecting over 3 million Americans. This disease can lead to esophageal adenocarcinoma, a highly lethal cancer. By analyzing Barrett’s esophagus cells over six years, the researchers found that genetic instability and chromosomal aberrations are key indicators of the cancer’s progression.
The study revealed that the diseased tissue often originates from a single altered ancestral cell and that genetic diversity in biopsies can predict cancer risk. This research provides crucial insights into the evolutionary dynamics of cancer development, potentially improving diagnostic and treatment strategies for Barrett’s esophagus, adenocarcinoma, and other cancers.
DNA milestones
The Biodesign Institute is also at the forefront of DNA nanotechnology research, producing advancements ranging from ultra-tiny electronics to revolutionary medical therapeutics.
Acute kidney injury is a severe medical condition affecting millions annually, often leading to high mortality rates due to the rapid accumulation of waste products in the blood. Currently, no effective cure exists for this disease, making it a significant challenge in modern medicine.
Biodesign researchers have developed a new approach using DNA origami nanostructures to treat and prevent acute kidney injury. These tiny, self-assembling forms — composed of DNA folded into complex shapes — are designed to accumulate in the kidneys. Biodesign researchers have demonstrated their promise in protecting healthy kidneys and improving kidney function following damage.
In experiments conducted on mice and human embryonic kidney cells, DNA origami nanostructures were shown to be as effective as the leading antioxidant drug in alleviating oxidative stress, a major cause of this disease. Positron emission tomography (PET) imaging revealed that rectangular nanostructures were particularly effective in protecting kidneys, marking a significant advancement in nanomedicine. This research paves the way for new therapeutic approaches and underscores the promise of DNA nanotechnology for a broad range of medical applications.
“This research marks a significant breakthrough in how we approach the treatment of acute kidney injury,” says Hao Yan, lead author of the study and director of the Biodesign Center for Molecular Design and Biomimetics. “This study not only underscores the potential of nanotechnology in medicine but also highlights the importance of interdisciplinary collaboration in overcoming some of the most challenging medical conditions. As we move forward, this approach may pave the way for new therapies that improve patient outcomes and revolutionize how we treat renal diseases.”
At Biodesign, DNA nanotechnology is also being used to create ultrahigh-density nanoelectronic systems. Researchers in the Biodesign Center for Bioelectronics and Biosensors are developing a manufacturing process using DNA nanostructures as scaffolds to organize nanoelectronic components like carbon nanotubes and nanoparticles. This approach aims to integrate these nanoscale parts with conventional silicon-based circuits, achieving unprecedented densities in hybrid electronic systems.
Funded by a $3 million grant from the National Science Foundation, this project explores the potential of DNA nanotechnology in electronics, aiming to produce highly sensitive and selective biosensors for detecting specific biomolecules. Such advancements could revolutionize medical diagnostics, food safety monitoring and biodefense. Additionally, the modular and reprogrammable nature of the platform promises versatile applications in future nanoelectronic systems.
One of the most innovative applications of DNA nanotechnology is the creation of robotic walking devices made of DNA strands that move stepwise along a path. This method, which allows DNA segments to traverse a defined area, is called strand displacement. In a DNA nanotech tour de force, ASU researchers have designed a high-speed DNA walker capable of rapid movement across a prepared track. The DNA walker moves by cartwheeling head over heels, covering ground 10 to 100 times faster than previous devices.
The walker’s unique locomotion, inspired by kung fu acrobatics, enhances its speed and efficiency, making it a significant advancement in the field of DNA nanotechnology. By optimizing DNA strand lengths and sequences, the researchers achieved a stepping rate an order of magnitude faster than earlier models, showcasing the potential for further innovations in DNA-based nanomachines for industry and medicine.
New plant-based technologies
Researchers with the Biodesign Institute have also pioneered plant-based therapies, leveraging the natural properties of plants to develop effective, low-cost medical treatments and diagnostics.
Mosquito-borne diseases are increasingly prevalent in the United States, with West Nile virus (WNV) posing a major public health challenge. Traditional methods to diagnose the virus are expensive and difficult to scale. In response, researchers have developed an innovative plant-based diagnostic method. Using advanced plant biotechnology, they have engineered plants to produce biological reagents that detect this disease. This method offers a cost-effective and scalable alternative to traditional diagnostics.
Their research highlights the production of recombinant antigens and monoclonal antibodies in plants including tobacco and lettuce. Recombinant antigens are proteins engineered to mimic parts of viruses or bacteria to trigger an immune response, while monoclonal antibodies are lab-made proteins designed to bind to and neutralize specific targets, such as cancer cells. This approach improves diagnostic accuracy and offers affordable testing for West Nile virus in regions with scarce medical resources, including the developing world.
“Most current protein-based diagnostic methods cannot differentiate WNV infection from related flaviviruses like dengue and Zika,” says Shawn Chen, lead author of the study. “However, our test is specifically designed for WNV. It is affordable, fast and suitable for both clinical and at-home use, significantly improving diagnostic accuracy and ensuring appropriate treatment for WNV patients.”
In other research, Biodesign’s multipronged attack on COVID-19 includes the development of a plant-based treatment. This approach uses a process called “transient expression” in tobacco plants to produce a monoclonal antibody. This therapy has a significant advantage: It may offer protection against COVID-19, even as the virus mutates to evade immune detection. The treatment could be especially beneficial for elderly patients and those with compromised immune systems who are highly vulnerable to SARS-CoV-2.
The new therapy could be combined with existing COVID-19 treatments to enhance their effectiveness. Plant-based therapeutics offer additional benefits, including reduced cost, safety, and faster development times.
The first monoclonal antibodies developed in the 1970s targeted cancer and have since been adapted to combat a wide range of diseases, including COVID-19. Although most current monoclonal antibody therapies for COVID-19 use Class I or II antibodies, the new therapy uses a Class IV monoclonal antibody, providing key advantages over existing treatments. Monoclonal antibody treatment is largely mutation-resistant and can neutralize multiple variants, making it a valuable candidate for combating new mutations of the virus.
Finally, norovirus is a highly contagious disease that causes severe gastrointestinal illness. Despite its prevalence, there is currently no vaccine. However, researchers at the Biodesign Institute have developed a plant-based vaccine against norovirus by using tobacco plants to produce virus-like particles — structures that mimic the outer shell of viruses but do not contain any viral genetic material.
Their study outlines the production of these particles using the bean yellow dwarf virus as a vector. The plant-based system allows for rapid, high-yield production of virus-like particles, which are effective at stimulating an immune response without causing disease. This method offers a cost-effective and safe alternative to traditional vaccine production, with the potential to be scaled up quickly in response to outbreaks. An effective vaccine against gastroenteritis is estimated to save billions of dollars in health care costs in the U.S. alone.
These advancements in plant-based therapies underscore the Biodesign Institute’s commitment to developing innovative, sustainable and scalable medical solutions. Through interdisciplinary research and collaboration, the institute continues to push the boundaries of what is possible in the realm of plant biotechnology.
'20 Years of Discovery' at ASU's Biodesign Institute
Explore the other installments in this series:
More Science and technology

Applied Materials invests in ASU to advance technology for a brighter future
For nearly 60 years, global giant Applied Materials has been hard at work engineering technology that continues to change how microchips are made.Their products power everything from flat-panel…

Meet ASU engineering students who are improving health care, computing and more
Furthering knowledge of water resource management, increasing the efficiency of manufacturing point-of-care health diagnostic tools and exploring new uses for emerging computer memory are just some…

Turning up the light: Plants, semiconductors and fuel production
What can plants and semiconductors teach us about fuel production?ASU's Gary Moore hopes to find out.With the aim of learning how to create viable alternatives to fossil-based fuels, Moore — an…