ASU epidemiologist on the rise in US measles cases
Photo courtesy CDC, Allison M. Maiuri, MPH, CHES
The Centers for Disease Control and Prevention issued an alert this month about a rise in measles cases worldwide. And as of March 21, a total of 64 measles casesIn comparison, the CDC reported a total of 58 measles cases for all of 2023. were reported in 17 states, including Arizona.
“Like any infectious disease, measles is best managed through a combination of education, prevention, public health policy and rapid response to incidents,” said Aaron Krasnow, associate vice president of ASU Health and Counseling Services.
“ASU Health Services follows established guidelines for infectious diseases set by the Centers for Disease Control and the Arizona Department of Health. In the event that we or Maricopa County Department of Public Health (MCDPH) identify an outbreak, we work closely with the MCDPH to follow guidance to protect the ASU community and beyond.”
ASU News spoke with Megan Jehn, epidemiologist and professor at the School of Human Evolution and Social Change, about why we might be seeing an increase and how to stay safe.
Question: Why might we be seeing an increase in measles cases across the U.S. this year?
Answer: We see measles cases every year, so a case here and there is not abnormal. What is concerning is the high number of infections so early in 2024 and the slow and steady rise in cases over the last 10 years. Measles cases often originate from unvaccinated or undervaccinated United States residents who travel internationally and then return home and transmit the disease to people who are not vaccinated against measles.
One interesting thing about measles is that it is known to have epidemic cycles. It tends to flare up every four to five years — we saw big outbreaks in the U.S. in 2008, 2011, 2014 and 2019, which suggests that we might be in for a bad year this year.
I think there are a number of factors contributing to the increased number of cases that we are seeing. First, national trends suggest that fewer children are receiving state-required vaccinations, and we have the lowest measles, mumps and rubella (MMR) vaccination rates in over a decade. When measles vaccination rates are too low — below 95% — that gives measles an opportunity to make an entrance and spread in a community. We are at 89.9% for two-dose MMR coverage in Arizona, which is one of the lowest childhood vaccination rates in the U.S. The reasons for this are complex but likely driven by existing barriers to accessing health care (which have been exacerbated by the pandemic), lack of awareness, misinformation and some culturally driven vaccine hesitancy.
One other contributing factor is that as generations age, our collective memory of diseases common in the 20th century fades. Thanks to vaccines, most of us don’t know someone who has suffered from serious complications of measles. We have forgotten how dangerous measles can be, and some may even wonder why we still need to vaccinate for a disease that we don’t see very often.
Q: What do we know about current cases of measles and past cases here in Arizona?
A: Arizona is one of 17 states reporting measles cases so far in 2024. We have had four cases reported by Maricopa and Coconino counties in the last few weeks. Our last significant measles outbreak in Arizona was in 2016, when 31 cases were reported. Our state and local public health officials have worked hard to contain any outbreaks, but we need a cohesive and coordinated plan to improve childhood immunization rates moving forward to protect our community.
Q: In the U.S., we have had a status of measles elimination since 2000. What does that mean?
A: Thanks to widespread adoption of the measles vaccination over the last few decades, measles was declared eliminated from the United States in 2000. This means the disease is no longer constantly present (endemic) in this country. However, travelers bring measles into the United States and it can sometimes spread and cause sporadic local outbreaks. Our goal is to make sure that these imported cases don’t go beyond a small outbreak.
Q: What is your role as an epidemiologist? How do you help keep people safe?
A: A single measles case is a public health priority and results in a significant economic and personnel burden for public health systems. Epidemiologists are working hard behind the scenes to establish enhanced surveillance and data collection systems and implement control measures to slow transmission. Containing a measles outbreak hinges on rapid identification of cases followed by detailed case investigation followed by contact tracing and quarantine of susceptible individuals who have been exposed.
My role is primarily to serve as a liaison between local public health officials and university leadership to make sure that ASU is aware of the ongoing situation and is prepared to respond if necessary. Through the ASU Student Outbreak Response Team, which I direct, we also indirectly support the measles response by providing additional public health surge capacity for routine public health investigations so that local epidemiologists can quickly and seamlessly pivot to the measles response. If the number of cases exceeds local public health capacity, our student team will be ready to assist in any way that they can. Because the best way to slow the spread is to increase community vaccination rates, our job in public health is also to empower trusted messengers to communicate the seriousness of measles and the safety of the vaccine.
Q: Anything else you would like to add or want people to know?
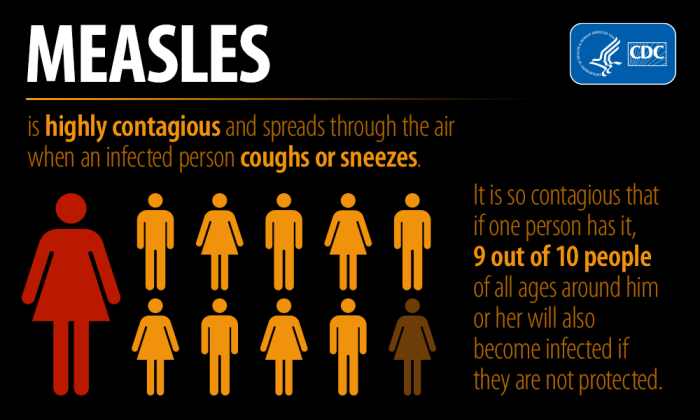
A: Measles is a highly contagious viral infection. It is so contagious that if one person has it, nine out of 10 people of all ages around him or her will also become infected if they are not protected. It is spread by coughing and sneezing or breathing the air that was breathed by someone with measles. The virus can linger in the air for approximately two hours. Given the currently high population immunity against measles in most U.S. communities, the risk of widespread disease is very low. However, pockets of low vaccination coverage leave some communities at higher risk for spread, so we expect to see additional cases and local outbreaks across the U.S. Those who are most vulnerable include babies too young to be immunized, pregnant women, immunocompromised people and those unvaccinated against measles.
It’s not “just a rash.” While most people who get measles will recover, it can be a devastating disease, and even mild cases can face longer-term health issues. About 30% of measles cases develop serious complications, including pneumonia, ear infections with potential permanent hearing loss, encephalitis and respiratory and neurologic complications that can result in death. The measles virus also has the ability to destroy immune memory from previous infections, inducing a type of immune system amnesia which can be very dangerous.
The risk of infection far outweighs the risk of the vaccine. The measles, mumps and rubella (MMR) vaccine is a safe and highly effective vaccine that can help people and their communities.
More Health and medicine
ASU team part of nationwide study looking at Type 2 diabetes in youth
Near the end of an interview in which he talked about the work his team will be doing to tackle the rise in Type 2 diabetes among youth, Arizona State University Professor Gabe Shaibi answered why…
Leading the way in wellness: ASU highlighted in The Princeton Review's 2025 Mental Health Services Honor Roll
Being a college student isn’t easy — navigating new routines, people and places can be a challenge, especially if the right support system is not in place. That's why Arizona State University is a…
New Indigenous health dashboard offers robust database for scholars
By Nicole Greason and Kimberly Linn A team at Arizona State University’s College of Health Solutions and American Indian Studies program has created a new tool to aid researchers…