The COVID-19 pandemic has been a major stressor for America’s health care system. While simultaneously losing revenue, hospitals saw massive surges in sick patients, shortages of equipment and staff, and massive burnout among their front-line workers.
Since last summer, Arizona State University has been part of a unique initiative to get health care delivery systems in Maricopa County to collaborate to improve patient outcomes — even though they are sometimes competitors.
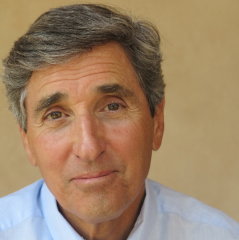
Denis Cortese, director of the Center for Healthcare Delivery and Policy at ASU, has led the effort. Cortese, former president and CEO of Mayo Clinic, described the work during the 2021 McKenna Lecture on March 9. The annual event, livestreamed this year, was sponsored by the Health Sector Supply Chain Research Consortium in the W. P. Carey School of Business at ASU.
“The pandemic is a common enemy where we have the chance to bring disparate systems together, which ordinarily are quite competitive, and see what we can do to improve care under circumstances of great stress,” said Cortese, who is a physician, Foundation Professor in the College of Health Solutions at ASU and president of the newly launched Healthcare Transformation Institute, based in Phoenix.
Denis Cortese, director of the Center for Healthcare Delivery and Policy at ASU, is leading an effort to get hospitals to collaborate.
Last summer, Cortese called the CEOs of several hospital systems in Maricopa County to gauge their interest in collaborating to improve health care during an emergency like a pandemic — and beyond.
“The goal was to build an orchestra that makes the right kind of music. I started with the chamber orchestra — the CEOs — because without them, it doesn’t work,” he said.
“We have a lot of delivery systems who are outstanding soloists, but the goal was to get them to work together and not maximize their own sector.”
CEOs of eight systems expressed interest in collaborating: Abrazo, Banner Health, Dignity, HonorHealth, Mayo Clinic, Phoenix Children’s Hospital, ValleyWise Health and the VA Hospital.
Cortese asked the CEOs to categorize and then rank their hospitals’ problems. A good foundation of work was done before everyone even met for the first time.
“They were viewing us as a neutral body to be the coordinator and to bring people together,” he said. “We’re not going to own anything or drive anything.
“The ASU Center for Healthcare Delivery and Policy program is the catalyst.”
The CEOs listed strategic objectives in three categories: supply chain (PPE, testing, ventilators), facilities (post-acute care, bed capacity, telehealth) and workforce (staff, licensing, burnout). One of the biggest problems they mentioned was post-acute care.
“Post-acute care is moving people out of the ICU who still need ventilator support and dialysis. This community doesn’t have a facility that can manage people post-acute care.
“This was a big, important factor for the hospitals (during the pandemic surge) because the ICUs were beyond capacity because they couldn’t move people out. The bathtub was filling faster than the drain was letting water out.”
Workforce training and readiness are also big issues.
“It means training physicians and nurses to do things that no one has trained them to do,” he said.
“Just going into a hospital for an outpatient doctor or nurse is tricky because they have to learn the electronic systems.”
Work on the collaborative had to be paused during the surge in COVID-19 cases in January and February. But now the team is working with the systems’ chief medical officers to untangle supply-chain issues.
“The delivery systems themselves need a better idea of how their supply chains go, down to who gives the injections,” he said.
One outcome of the pandemic is the heightened realization of how the supply chain is interconnected and where it’s failed.
“We had an example in the last two or three years where hospitals collectively went together in Utah and built their own pharmaceutical company to supply generics,” he said.
“They decided to take control of their own supply chain. We need to be prepared to go that far.”
At some point, the collaboration will bring in public health departments, and eventually, consider research and educational opportunities, he said.
Cortese said the hospitals had already been collaborating to manage emergent patient care during the surges and responded quickly when needed.
“What happened was that the state wasn’t prepared at all at the public health level,” he said.
“The delivery systems stepped in and pulled people off their front lines to give the injections. The fact that Arizona has done as well as it’s done is because the delivery systems stepped in.”
Cortese said he doesn’t know what the collaboration will eventually look like. While the initial group is eight hospital systems, Cortese knows that not all might continue, but that others will likely join in the future and that the vision is long term.
“I’ve done this work before in my career,” he said. In the 1980s, when he was with Mayo Clinic in Minnesota, he was part of a collaboration with four hospital groups to improve patient outcomes.
“It took us five years of meeting and debating because we all walked in with the attitude that we knew what we were doing and nobody was better than we were and why should we cooperate.
“Then we started looking at our own results, and how we were progressing. Then the tone changed.”
The initial collaboration led to a nonprofit organization that measures outcomes and costs of primary care in Minnesota.
“And 30 years later, every hospital in the state participates,” he said.
While the current effort started in response to an emergency, the goal is for the collaborative to endure for future disasters.
“We have to do this long term. I’m tired of hearing that this is a once-in-a-century event,” Cortese said.
“We had Zika. We had H1N1. We had Ebola, which could have blown up on us.
“And we weren’t ready for any of them.”
Top image courtesy of Pixabay.
More Health and medicine

10 companies, 5 nations, 1 accelerator: A wide range of innovative health care solutions
The 10 companies participating in the 2025 Mayo Clinic and ASU MedTech Accelerator program hail from five different nations and are the first cohort to have representation from life science companies…

'Incredible milestone': ASU, city of Phoenix announce location for ASU Health headquarters
Citing the need for a “new way” of doing things, Arizona State University President Michael Crow said that the headquarters for ASU Health will be the hub of the university’s efforts to improve…

Have a health question? This newsletter is for you
You sprain a knee while playing basketball. Your stomach hurts all the time. You keep getting bad headaches.What’s the first thing you do, besides making a doctor’s appointment?If you’re like most…