As with many complex maladies, a deep understanding of Alzheimer’s disease has been elusive for the simple reason that a variety of physiological, biological and chemical factors — acting either singularly or in combination — could reasonably be conjectured to cause the disease.
Efforts are increasing to more precisely identify which factors are to blame. Those endeavors now include federally funded research by Michael Sierks and Ping He at Arizona State University, which is viewed as a potentially significant step toward zeroing in on factors that do play a role in triggering Alzheimer’s onset.
Sierks is a professor of chemical engineering in ASU’s Ira A. Fulton Schools of Engineering, and He is an associate research scientist in the Fulton Schools.
Their research paper, recently published in the Journal of Biological Chemistry, earned recognition as one of the publication’s editors’ picks for the importance of its findings.
Alzheimer’s, an irreversible brain disease, is the most common cause of dementia, and is estimated to afflict at least 1 in 10 people age 65 and older, and about 3 in 10 people age 85 and older.
Research led by Michael Sierks, a Fulton Schools professor of chemical engineering, focuses on antibody-based therapeutics for treating neurodegenerative diseases such as Alzheimer’s and Parkinson’s diseases.
Sierks and He’s efforts have focused on closely examining proteins and peptides that are typically found in the brains of Alzheimer’s patients. They’re looking for specific kinds of toxic conformations of these proteins and peptides that are in specific locations in the brain.
Previous research has shown that when levels of the amyloid beta protein accumulate in the brain and are not properly cleared out, the protein can clump together between neurons (nerve cells) in the brain to generate various aggregates — including small soluble aggregates and larger insoluble amyloid plaques that are a hallmark of Alzheimer’s. It’s suspected that small toxic soluble aggregates lead to neurodegeneration as a precursor to the onset of Alzheimer’s.
Sierks and He experimented with targeting specific forms of the amyloid beta protein using novel antibodies generated in their lab to study the potential effects of targeting specific toxic protein conformations in a mouse model of Alzheimer’s.
They found that targeting one specific toxic form of amyloid beta restored neuronal integrity — meaning that neurons are intact and undamaged — in the mouse model, which could conceivably reverse or inhibit dementia.
Targeting the specific beta amyloid variant also dramatically reduced the presence of activated microglial cells, an indicator of potential problems in the brain. It’s an inflammatory process in the central nervous system thought to contribute to neuronal cell death in a number of neurodegenerative diseases, including Parkinson’s disease, Alzheimer’s, multiple sclerosis and HIV-dementia.
Sierks says his and He’s investigations looked at how targeting toxic amyloid beta proteins generated either inside or outside brain cells can affect the progression of Alzheimer’s.
Their findings indicate that earlier attempts to treat the disease may have failed because researchers were focusing their attention on the wrong things, says Sierks, who teaches in the School for Engineering of Matter, Transport and Energy, one of the six Fulton Schools.
So, previous failed clinical trials may have missed detecting and targeting the key protein species causing brain degeneration, Sierks says. Those trials instead focused on other protein species that are also present in cases of Alzheimer’s but that may not be active in the biological and chemical processes leading to the disease.
Sierks and He want to set the stage to accomplish more than increasing knowledge about the causes of the disease.
“If we can learn a lot more about the causes, that is going to give us a good idea of what direction to go in to develop better therapies for controling Alzheimer’s,” Sierks said.
The two researchers see the potential for progress in their efforts to provide a foundation for personalized medicine approaches to dealing with the disease.
“Everybody’s cancer is different. In the same way, everybody’s Alzheimer’s or dementia is different,” Sierks said. “We are hoping we can help lead the way to someday being able to target therapy to individuals based on specific differences in their conditions.”
There’s a long way to go to bring that advance into sight, the researchers say. They are confident that their approach is ready to be tested in clinical trials, but that will require substantial funding.
The plan now is to team with pharmaceutical research enterprises, or maybe even form a startup, and then seek financial support from government sources — most likely the National Institutes of Health — and perhaps from private and industry investors as well.
To be successful, the venture will require sufficient resources to bring together other experienced researchers along with physicians, clinicians, therapists and other medical specialists with expertise in Alzheimer’s, dementia and related health conditions.
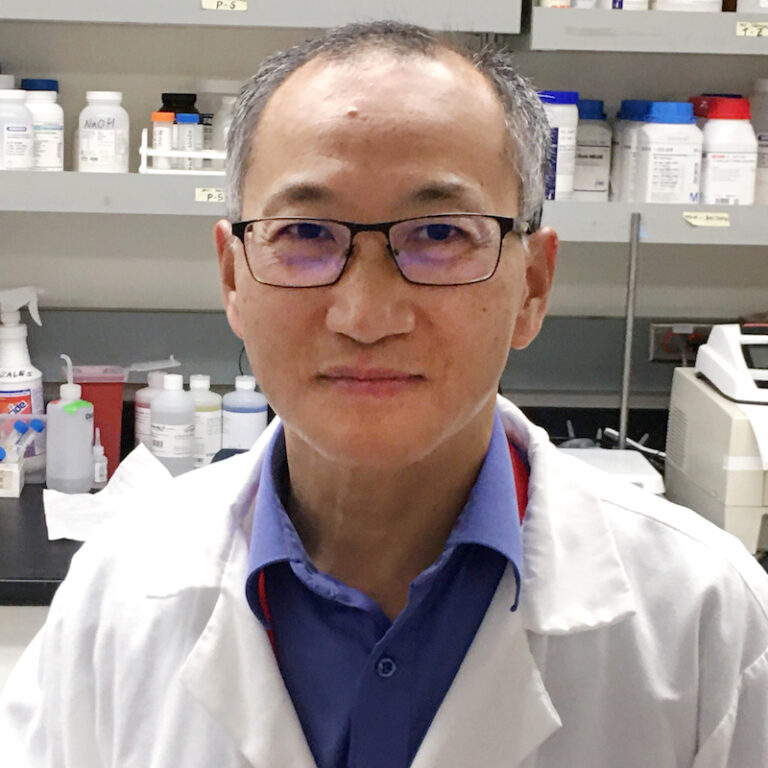
Fulton Schools Associate Research Scientist Ping He performed the experimental design, brain imaging, statistical analysis, data interpretation and related work in recent research pursuits that have resulted in important new information about the onset of Alzheimer’s disease. Photographer: Philip Schulz/ASU
Their mission will be to develop an antibody designed to shield against the accumulations of the most neurotoxic forms of the amyloid protein that may lie at the heart of early stages of Alzheimer’s, and to do this before the disease has progressed and caused irreversible brain damage.
Sierks credits He for performing the lion’s share of work necessary to justify undertaking the ambitious venture.
He did the experimental design, immunohistochemistry, brain imaging, ELISA analysis, statistical analysis and data interpretation for their research, and also drafted and revised the research paper manuscript.
“We are aiming to take a different approach from what others have done,” Sierks said, “and He really helped to put us into a position to make a strong case for doing this.”
Other experts agree the results of the research convincingly show the project is deserving of support for further development and testing.
For instance, the paper’s description of the toxic nature of intracellular amyloid oligomers in the published research paper gives credence to a hypothesis derived from earlier research at a Harvard University lab led by amyloid hypotheses pioneer Dennis Selkoe. This is according to Sierks’ colleague, Diego Mastroeni, an assistant research professor in ASU’s School of Life Sciences who also works in the ASU-Banner Neurodegenerative Disease Research Center.
Pharmaceutical companies, however, didn’t fully explore the potential impact of that research. But now, Mastroeni says, the Selkoe lab’s contributions can be validated by the new data from Sierks’ and He’s work, which “strongly suggests that the amyloid hypothesis is not doomed for failure, we just need to target the right variant in the right place.”
Eliezer Masliah, director of the Division of Neuroscience for the National Institute on Aging, a part of the National Institutes of Health, noted in particular that the ASU researchers have produced antibodies — important parts of the immune system — that can recognize different types of amyloids.
That ability would enable identifying the most potentially harmful amyloid accumulations and targeting them for removal, thereby reducing the spread of cell injury and inflammation, said Masliah, who leads NIH-sponsored programs aimed at better understanding brain aging and Alzheimer’s disease.
The research “solidly suggests that it’s important that we use these antibodies that can actually penetrate into the neurons to remove amyloid accumulations,” Masliah said, noting that Sierks and He also cleverly made use of a protein fragment that “acts like a Trojan horse and actually tricks the neuron into taking in the antibody.”
The research featured in this article was funded in part by grants from the National Institutes of Health (R01AG054048, S10RR027154)
More Science and technology

Teaching construction realities with virtual environments
Visiting a construction site is a valuable learning opportunity for students who want to one day work in the industry.…
ASU, Mexico partner to build next generation of chipmakers, drive semiconductor innovation
Thousands of college students in Mexico will soon have the opportunity to enroll in Arizona State University’s new, free online…
ASU, St. Mary’s Food Bank partner to tackle food insecurity in Arizona
Arizona State University and St. Mary’s Food Bank (SMFB) have joined forces to create an interactive data dashboard that tracks…