ASU, Mayo Clinic and Maricopa County Department of Public Health collaborate on antibody survey

Maricopa County Department of Public Health, Mayo Clinic and Arizona State University are embarking on an ambitious project to better understand the prevalence and spread of COVID-19 cases in the county — and they need the public’s help to do it.
Their Serosurvey Project will send teams across the Valley of the Sun to selected neighborhoods and request blood samples from residents for antibody tests to determine if households had any prior exposure to COVID-19. In the absence of the ability to currently test everyone, such a survey will provide critical insights for the county health department (MCDPH) to better understand and project how many Maricopa County residents may have already been infected with the SARS-CoV-2 virus.
“It will be really eye-opening to get an idea of how much spread we actually have had in Maricopa County,” said Marcy Flanagan, executive director at MCDPH. “Our residents have been great at stepping up to help reduce spread and protect our families, friends, and neighbors, and participating in this serosurvey is a way to contribute to knowledge specific to our community.”
The sample collection and survey of Maricopa County residents will run from Sept. 12 to Sept. 20.
Why Maricopa County health needs your help
The project aims to collect 500 samples from 210 households in selected clusters throughout Maricopa County. The clusters were chosen using a Centers for Disease Control and Prevention technique called Community Assessment for Public Health Emergency Response (CASPER). CASPER is designed to give public health officials a snapshot of a community based on a carefully selected sample representative of the larger population. This can better inform public health strategies, identify information gaps, aid response and recovery, allocate resources and assess new or changing needs in communities.
The teams will go to people’s homes instead of relying on patients coming to a clinic for testing, because this method ensures a more accurate representation of the community, said Megan Jehn, an associate professor in ASU’s School of Human Evolution and Social Change. Jehn is an infectious disease epidemiologist who leads a student outbreak response team working with MCDPH to support the public health response to COVID-19.
“We're trying to come out on different days of the week, at different times of the day and to different neighborhoods, because we want everyone to be represented,” Jehn said. “We want to know the true impact of COVID-19 in the community with a sample to reflect our community’s socioeconomic, geographic, age and ethnic diversity.”
What antibodies tell us
Once collected, Mayo Clinic will test the blood samples for antibodies, which are proteins that our bodies produce in a unique response to a particular germ.
“The process of making antibodies starts with exposure to a virus — your body sees that virus, recognizes it as foreign and will generate antibodies against it,” said Erin Kaleta, director of Infectious Disease Serology and co-director of Clinical Chemistry at Mayo Clinic. Kaleta will be leading the sample testing.
A negative test result means that an individual has probably not had the virus, while a positive result means someone was probably infected with COVID-19 at some point in the past. And studies have shown that even people who may be asymptomatic for COVID-19 can produce antibodies to the virus.
Since this antibody data shows who has and hasn’t been infected, it gives public health officials a more accurate idea of the actual number of cases in the county. The serosurvey will allow MCDPH to calculate an estimated total number of undiagnosed cases for Maricopa County. Similar projects in the U.S. found that for every diagnosed case of COVID-19, as many as eight to 10 people had antibodies. This suggests the virus is far more prevalent than diagnostic testing reveals.
“The benefit of this is that we can get a better idea of who's been infected overall, which is a better indicator than using diagnostic testing, as those only see a moment in time,” Kaleta said.
In addition to aiding the county’s public health work, the antibody data could provide useful information to participants volunteering blood samples.
“You might learn something about how your behavior is associated with your likelihood of contracting COVID-19,” Jehn said. “You may learn something about those risk factors that you have in your life.”
First county household demographic data
Along with blood samples, teams will be conducting a survey with residents to gain a more complete picture of each household’s experience with COVID-19.
The survey questionnaire will provide data on a household’s experience with COVID-19 testing and quarantine, chronic illnesses, employment and access to health care, and finally knowledge, attitudes and household practices related to COVID-19.
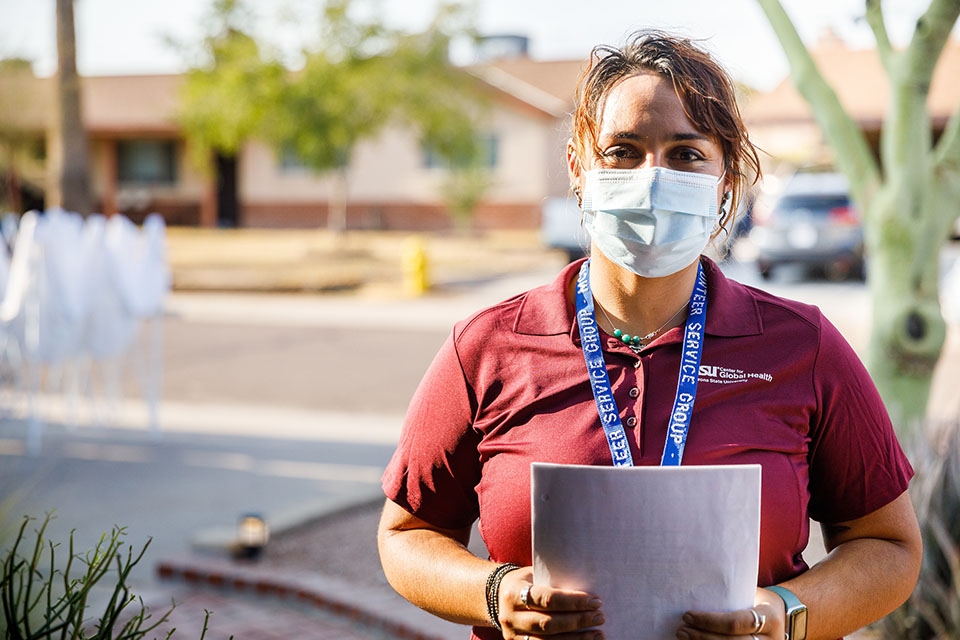
Survey questions will be asked at the same time as the blood draw, which will be collected by nursing students from ASU’s Edson College of Nursing and Health Innovation, said Heather Ross, an assistant professor in the Edson College, who aided the survey development.
Ross is also working to staff the serosurvey field teams with ASU students in global health and anthropology programs. In addition, volunteers who support Maricopa County Department of Public Health’s efforts will serve in a variety of roles, both in the field teams and behind-the-scenes.
“The most critical component of this project is field teams asking residents for blood samples,” said Michael Shafer, a professor in the School of Social Work in the Watts College of Public Service and Community Solutions. “That’s a pretty big lift.”
To ease the load, field teams will be partially staffed with students in social work programs, who bring a useful skill set to the Serosurvey Project.
“Social work students can empathize, build rapport with residents, respond to fluid situations, and will be able to address people’s concerns in a constructive way,” Shafer said. “This is the kind of project that really galvanized me as a young man and taught me about what was important to me.”
Field teams will ask survey questions and collect blood samples in portable tents set up outside with the permission of participating residents, and a mobile clinic will be on hand for support. Team members will wear CDC-recommended personal protective equipment including masks, gloves, gowns and booties when conducting the surveys and drawing blood.
“This is to protect our field teams, but also to provide assurance of protection to a family who is inviting a stranger into their community in the name of public health,” Ross said.

Illustration by Ashley Quay.
Privacy is a priority
Privacy is just as important to the serosurvey team as accuracy. No personal identifying information will be attached to blood samples for testing. Instead, samples will be assigned codes when they are sent to Mayo Clinic. After testing, Mayo Clinic will return the results to MCDPH, who will match the codes with the participants before contacting the participants by phone. Participants can also request a mailed copy of their antibody test results.
“The thing that's really, really important to know about this is that all of the survey results and all of the blood test results will remain confidential,” Ross said. “They'll be shared with the county public health department. And that's it.”
Armed with that data, MCDPH can more effectively chart a course forward for Maricopa County. This is even more important as schools, businesses, places of worship and other community entities seek guidance on reopening safely.
Top photo: The blood draw will be collected by nursing students from ASU’s Edson College of Nursing and Health Innovation. Photo by Andy DeLisle
More Science and technology

ASU-led space telescope is ready to fly
The Star Planet Activity Research CubeSat, or SPARCS, a small space telescope that will monitor the flares and sunspot activity of low-mass stars, has now passed its pre-shipment review by NASA.…

ASU at the heart of the state's revitalized microelectronics industry
A stronger local economy, more reliable technology, and a future where our computers and devices do the impossible: that’s the transformation ASU is driving through its microelectronics research…

Breakthrough copper alloy achieves unprecedented high-temperature performance
A team of researchers from Arizona State University, the U.S. Army Research Laboratory, Lehigh University and Louisiana State University has developed a groundbreaking high-temperature copper alloy…