ASU study shows prediabetics may be 'exercise resistant'

In a recent study, School of Life Sciences Associate Professor Christos Katsanos discovered that obesity associated with prediabetes changes mitochondria in skeletal muscle, altering the way exercise affects their ability to burn fat. Photo by: Pixabay
Obesity is the single largest cause of diabetes. And the advice to solve it is often the same: Get off the couch. Hit the gym. Run around the block.
However, for people who are both prediabetic and obese, exercise may not actually help them counteract the negative effects of obesity on diabetes, according to a new study by Arizona State University School of Life Sciences Associate Professor Christos Katsanos.
The problem is in the mitochondria. Also known as the powerhouse of the cells, the mitochondria are the parts of the cells where you get the energy for your heart to beat, your brain to function and your skeletal muscles to move. Mitochondria make it happen.
Katsanos has a laboratory at Mayo Clinic in Arizona where he collaborates with faculty who study metabolism in diseases such as diabetes. At Mayo Clinic, his then-graduate student Katon Kras, discovered that for people who are prediabetic and obese, proteins, which are the building blocks of mitochondria, are modified in a way that is not optimal for them to process fats and glucose. This negates the ability of skeletal muscle to create enough energy, such as that used for muscle movement. Their findings appeared in the scientific journal Metabolism Clinical and Experimental.
Since diabetes cannot be reversed, Katsanos and Kras are striving to understand the prediabetic condition, hoping to find answers that may slow or stop the onset of diabetes. Could exercise be the answer?
They asked that question in another study published in Medicine and Science in Sports and Exercise in March 2019 and were surprised by the answer.
“Exercise did not stimulate the mitochondria of these people to produce enough energy,” Katsanos said. “We call these people ‘exercise resistant.’ It goes against the hypothesis that we had when we started. We’ve long believed exercise to be a solution to obesity.”
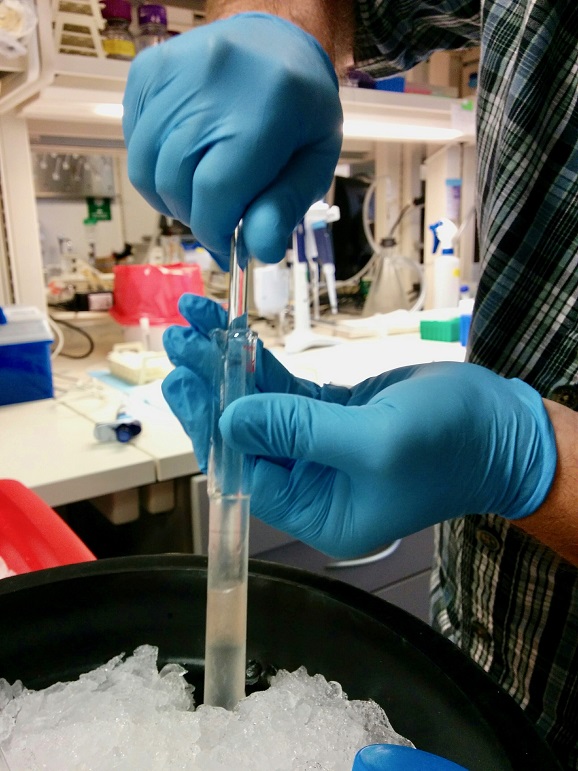
Katsanos and his graduate student Katon Kras biopsied tissues from healthy and prediabetic individuals and identified differences in mitochondria. Photo by Christos Katsanos/ASU
Katsanos and Kras looked at changes in the skeletal muscle of both obese and nonobese individuals after 45 minutes of exercise on a stationary bicycle. They studied two different populations of mitochondria: those found in the fibers of the skeletal muscle that cause them to contract and those found near the surface of the muscle tissue in the plasma membrane.
This produced novel results. Simply riding the bicycle for 45 minutes was enough to see measurable changes in the mitochondria of both groups. However, while there were no significant differences in how the contractile mitochondria responded, there were important differences in the response of surface mitochondria. Both types of mitochondria responded in nonobese individuals, but the surface mitochondria were impaired in obese individuals.
“It appears that obese people may be able to produce sufficient energy by contractile mitochondria to move around, to exercise,” Katsanos said. “What we saw was mitochondria that support metabolic functions of the cell under the plasma membrane are affected in obese individuals. And these are metabolic functions that are directly linked to diabetes.”
Kras compared the results to differences that we might observe in driving a race car versus a Yugo. Both contain engines that run the car (mitochondria), but the race car responds quickly to small changes while a cheaper car might not.
“The mitochondria coming from the skeletal muscle of a lean person seem to respond. If you touch the gas pedal, just a little bit, and the car goes. There’s a big change in the performance of the car. Where the other car, even if you stomp on the gas, the car just doesn’t go,” Kras said. “That’s what we were seeing in the mitochondria. We were giving it fuel, the same fuel to oxidize, and those mitochondria just didn’t respond the same way.”
Both obese and nonobese individuals may have the same ability to produce energy, but when you stimulate mitochondria from the different populations, you get lower response in the obese individuals.
Kras said that’s likely because the mitochondria in the obese person are already at the max and have no capacity to take on the extra workload. Individuals who are lean have lower baseline energy production, so there is room for the mitochondria to respond.
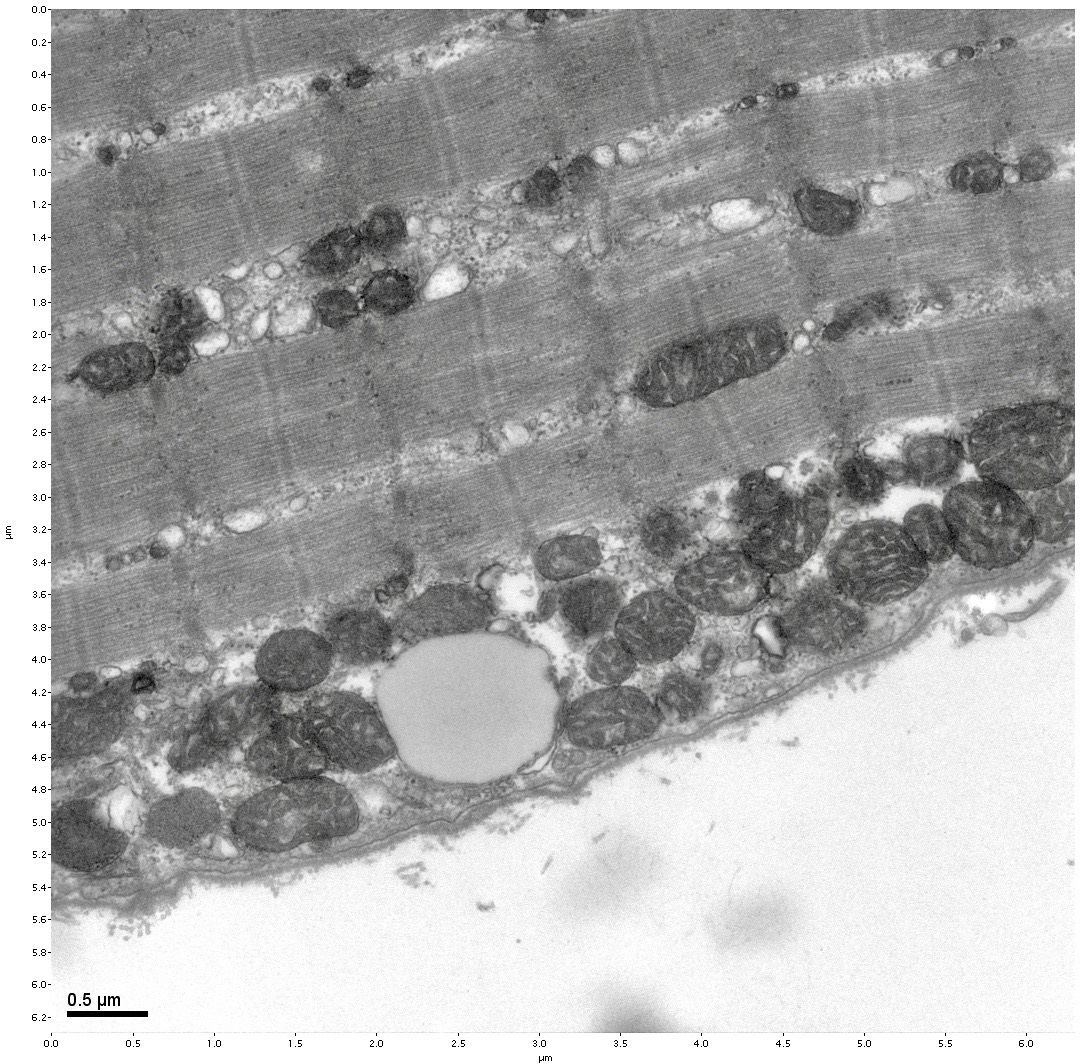
While the mitochondria within the skeletal muscle was similar between populations, Katsanos and Kras discovered that mitochondria near the surface did not respond to exercise in prediabetic individuals. Photo by Christos Katsanos/ASU
Understanding how mitochondria respond — and what treatments might be available to fix this — is becoming an increasingly important issue.
Worldwide, obesity is trending upwards and over the past four decades, has nearly tripled. According to the World Health Organization (WHO), more than 1.9 billion adults were overweight in 2016 — 650 million of those were considered obese.
WHO also reported in the same year more than 41 million children under age 5 and 340 million children and adolescents were overweight or obese.
Obesity is a major risk factor in developing diseases such as diabetes, cardiovascular diseases, cancer and musculoskeletal disorders, as well as causing disability and premature death.
“It’s hard to imagine how long the obesity epidemic will be trending upwards, but so far, it does not appear to be losing steam,” Katsanos said. “Where do we go from here? Is it realistically reversible, or can we undo its negative impacts on health? Those are the tough questions. If we had the answer, we’d be working toward it faster.”
Part of the problem was that research on the mitochondria in prediabetics have produced conflicting results. Kras and Katsanos tackled this problem in a way that hadn’t been done before: by separating the mitochondria into different populations and learning more about how each responds.
This led to the first discovery of differences in the proteins that make up both contractile mitochondria and surface population mitochondria in their 2018 study. In 2019, they took a novel approach to understanding the differences: Don’t just study the mitochondria. Study them after they have been stressed by exercise.
“It is easier to identify a possible defect when you stress the system. Like a car. If you put it out on the road and you put your foot on the gas pedal, you can see how good it is,” Katsanos said. “When a car is sitting, which is where most people have focused their research, it’s harder to see whether it’s good or bad.”
But they unearthed an interesting dilemma: the solution we always believed was available may not always work. As Kras points out, this complicates the story. If exercise isn’t the answer, what is?
“Lifestyle interventions may not be enough to regulate weight and energy metabolism in people who are obese. We’re telling them to just get up and move, but this may not necessarily be the answer,” Kras said. “Personalized management plans need to be looked at. We need to think about each individual person and try to figure out the mechanisms behind what’s leading to obesity because it really is still foggy.”
More Science and technology

Applied Materials invests in ASU to advance technology for a brighter future
For nearly 60 years, global giant Applied Materials has been hard at work engineering technology that continues to change how…

Meet ASU engineering students who are improving health care, computing and more
Furthering knowledge of water resource management, increasing the efficiency of manufacturing point-of-care health diagnostic…

Turning up the light: Plants, semiconductors and fuel production
What can plants and semiconductors teach us about fuel production?ASU's Gary Moore hopes to find out.With the aim of learning how…