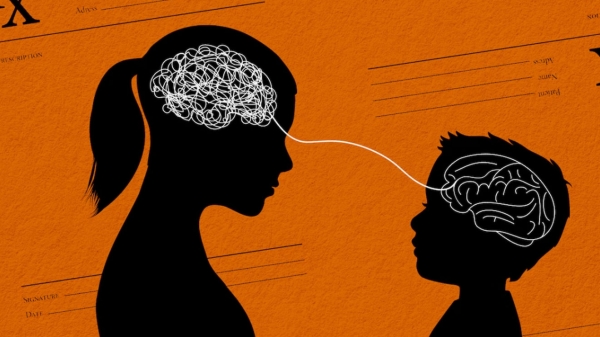
ASU researchers find heart rate variability in children affects long-term effects of maternal postpartum depression

Yessenia Moreno, a researcher in the ASU Department of Psychology, measures the respiratory sinus arrhythmia (RSA) in 12-week-old, Wesley Jewell.
Each year, approximately 10–15 percent of postpartum women suffer from postpartum depression, which translates into almost 1 million women. Women from low-income and ethnic minority families have disproportionately high rates of postpartum depression, which puts their children at risk for a wide range of behavioral problems during their lifetime.
Scientists in the Arizona State University Department of Psychology have discovered biological characteristics of young babies can forecast how vulnerable they might be to their caregiving environment. The researchers measured infant vagal toneActivity in the vagus nerve, a fundamental component of the parasympathetic branch of the autonomic nervous system., a noninvasive indicator of cardiovascular function, at 6 weeks of age and found it predicted how maternal postpartum depressive symptoms affected the child’s behavior at 3 years. Children with low vagal tone fared worse when their mothers suffered from more postpartum depressive symptoms. The findings will be published in Child Development on July 18.
A biomarker for resilience?
ASU psychology graduate student Jennifer Somers, the lead author on the study, wanted to know if biological factors could explain how the caregiving environment during infancy affects children as they develop.
“We know children are affected unequally by maternal postpartum depressive symptoms, and our goal was to start to understand which kids are more susceptible,” she said. “Little is known about how biological factors influence risky behavior and resilience among ethnic minority children raised in impoverished environments.”
The experiment was a longitudinal study of 322 low-income, Mexican-American families. It is part of a larger study called Las Madres Nuevas that focuses on what predicts postpartum depression in low-income ethnic minority women, who are at higher risk. The researchers asked how biological factors during the earliest phases of a child’s life and maternal postpartum depressive symptoms jointly contributed to children's behavior problems at ages 2 and 3.
“It is so important to understand for whom and under what circumstances depression in mothers is associated with negative effects on children’s functioning and what might explain those associations,” said Sherryl Goodman, professor of psychology at Emory University. Goodman is an expert on the effects of postpartum depression in children and was not involved with the study. “This study has important implications for theory, particularly in terms of understanding variability in the strength of association between depression in mothers and child functioning.”
When a less variable heart-rate is a good thing
To test whether characteristics of a child’s cardiovascular system might buffer against the effects of postpartum depressive symptoms in the mother, the researchers measured the respiratory sinus arrhythmia (RSA) in 6-week-old infants. The RSA indicates how variable the heart rate is and is easily and noninvasively measured using electrocardiography.
Also at 6 weeks postpartum, the depressive symptoms of the mother were assessed using the Edinburgh Postnatal Depression Scale, a standardized measure of postpartum depression. The mother’s depressive symptoms were assessed every three weeks until the baby was 6 months of age, to create a complete picture of the caregiving environment instead of a snapshot.
When the children were 24 months old, the mother and child visited ASU, where the researchers observed the mother-child pairs and noted how the child related to their caregiver.
“At age 2, toddlers should be able to use their caregiver to regulate their behavior, to adjust and adapt to new environments,” Somers said. “Postpartum depressive symptoms in mothers can have an enduring effect for some children and make them less likely to use their caregivers as a scaffold in situations where they need help to adapt.”
Three years after the study began, the mother provided a report on the child’s behavior. Children with less variability in their heart rate, or low RSA, showed more behavior problems when their mothers had postpartum depressive symptoms in the first six months. These same children fared better when their mothers reported fewer symptoms.
“The prevailing theory has been that higher RSA or vagal tone was associated with children being more vulnerable to their caregiving environment, but our findings suggest the opposite,” said Linda Luecken, professor of psychology and a principal investigator on the study. “Mothers in this study experienced mild-to-moderate postpartum depressive symptoms, so low vagal tone could be protective for infants with that kind of environmental exposure.”
Somers is hopeful the findings from this study can lead to more focused interventions for the children who need it most.
“Understanding how different caregiving environments affect the development of a child and the different ways a child might respond to their environment can help improve or create personalized interventions for children from high-risk populations,” she said.
Tracy Spinrad, professor in the T. Denny Sanford School of Social and Family Dynamics, and Keith Crnic, Foundation Professor of psychology, also contributed to the study.
More Science and technology
ASU graduate student researching interplay between family dynamics, ADHD
The symptoms of attention deficit hyperactivity disorder (ADHD) — which include daydreaming, making careless mistakes or taking…

Will this antibiotic work? ASU scientists develop rapid bacterial tests
Bacteria multiply at an astonishing rate, sometimes doubling in number in under four minutes. Imagine a doctor faced with a…

ASU researcher part of team discovering ways to fight drug-resistant bacteria
A new study published in the Science Advances journal featuring Arizona State University researchers has found…