ASU professor to extend potential benefits of rapid TB test to children

ASU Biodesign Institute researcher Tony Hu.
Recently, a new Arizona State University invention by ASU Biodesign Institute researcher Tony Hu has resulted in the development of the world’s fastest and most accurate blood test for tuberculosis (TB). The test can provide new hope to physicians in the treatment of people infected with TB, with results in a just few hours instead of the week or two it currently takes with traditional methods.
This new test, which Hu hopes to bring to the market soon, means patients who might have waited weeks or months to get the right drugs can now be diagnosed in a few hours. Doctors will be able to run the test early and often during therapy to see whether a patient’s treatments are working. This gives those infected with TB a greater chance of recovery.
Helping children
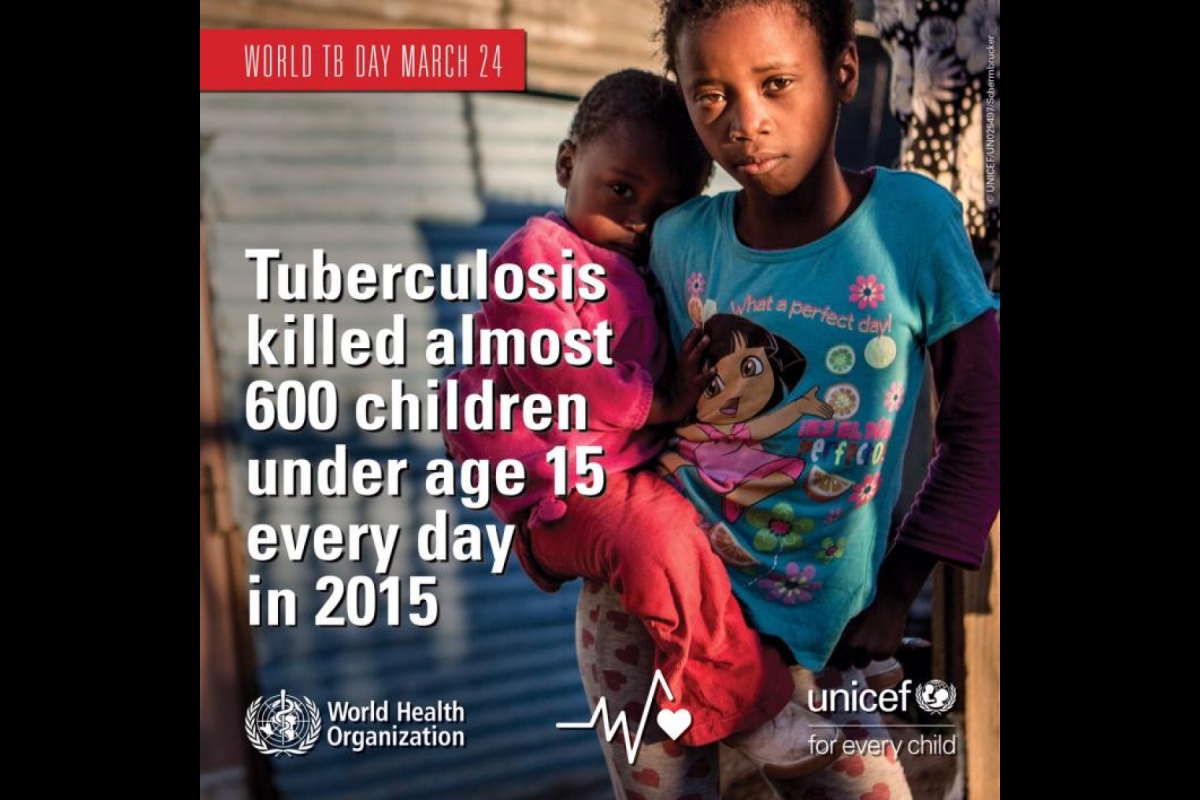
Tony Hu now wants to extend the vast potential of the test’s benefits to help save children infected by TB. This would be a potential game-changer for the one million children and ten million people who fall ill with TB every year.
Hu, a researcher at the Virginia Piper Center for Personal Diagnostics at ASU’s Biodesign Institute and faculty at the Ira A. Fulton Schools of Engineering, was recently awarded a five-year, $2.7 million grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to adapt his breakthrough technology and develop a new rapid tuberculosis diagnostic test for children.
“We are confident that our strategy will provide for the early detection of active pediatric TB cases, which will decrease TB disease progression and improve outcomes,” Hu said. “We also hope that rapid monitoring of pediatric TB therapy may allow physicians to personalize a child’s treatment to avoid unnecessary exposure to toxic TB drugs once a child has cleared their TB infection.”
Tuberculosis has historically been one of the most fatal diseases of the last couple centuries with about a billion deaths; it has historically been known as consumption or the white plague.
Part of the reason is that TB has cunningly evolved to survive within the human host undetected, living within one of the body's first lines of defense — immune cells. When the immune system is working as it should the infection is called latent, meaning the patient is asymptomatic but it can still be detected and treated.
Hu’s TB test is the first one that can rapidly and accurately identify the most dangerous, active stage of TB infections using a blood sample.
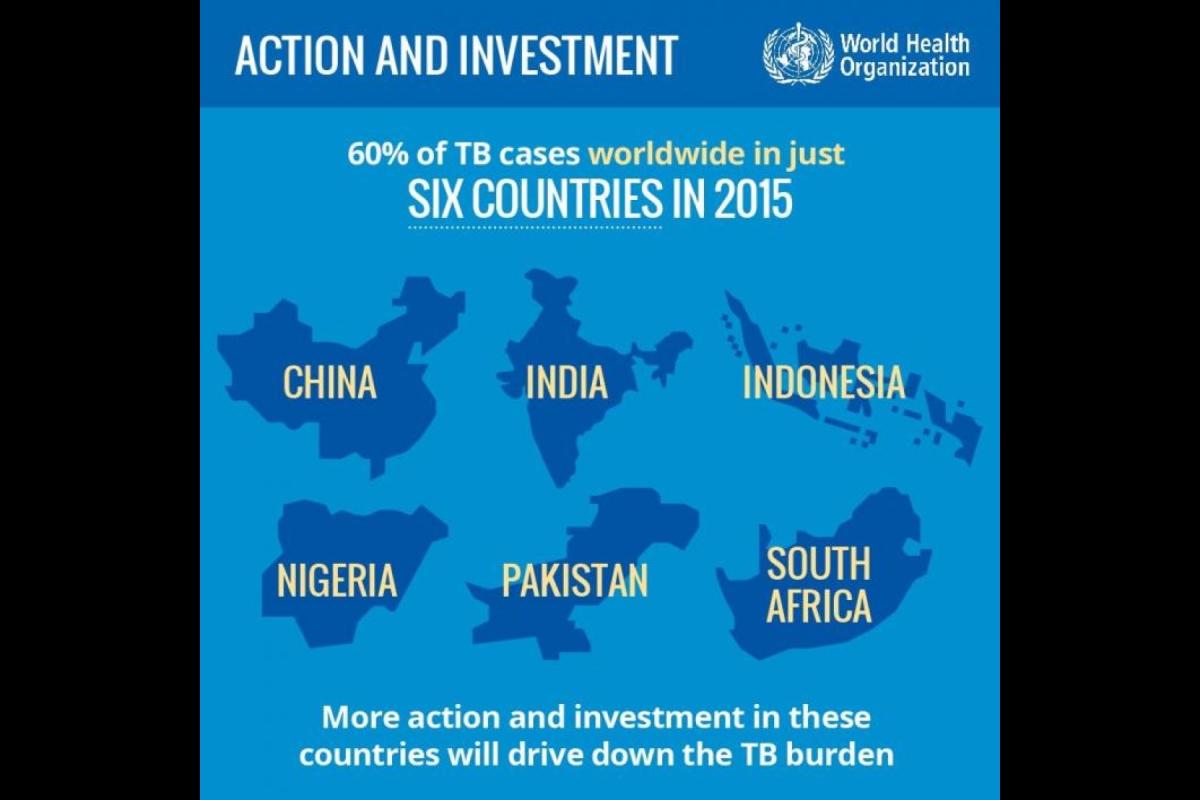
Although we have come a long way in our fight against tuberculosis, one-third of the world's population is still infected with TB today. According to the World Health Organization, in 2015, 10.4 million people around the world became sick and there were 1.8 million TB-related deaths worldwide — with an estimated 1 million children becoming ill and 170,000 children died from it.
Tuberculosis is a particularly dangerous disease for the young. Pediatric cases of TB have a particularly large rate of mortality and morbidity because children have not developed their immune systems fully and the disease can progress rapidly from latent to active TB.
The current testing methods are time intensive and sputum samples, the common way to confirm TB infection in adults, are difficult to obtain. Children often are infected with a smaller number of bacteria (paucibacillary disease) and can often falsely test negative.
It’s no wonder the World Health Organization has highlighted the development of a faster and more sensitive method for TB testing as a worldwide top priority.
Making an impact
The idea for the test sprung up when Hu was a chemist at the University of Texas Houston, working on new nanotechnology development — but he realized there were no known applications to the technology he was developing yet. He attended a biochemistry lecture that got him thinking about using it for diagnostics and decided to move into the biomedical engineering field seeing how his current skillset could be enhanced and applied for medically relevant purposes.
One of the hurdles they had to overcome was that biomarkers had not been detected in the blood before that were specific for active cases of TB. The team did extensive analysis on protein fragments and eventually found ones that made testing sensitive to even the difficult to detect cohorts like the commonly fatal HIV-TB co-infected.
“This exploratory work is in itself ground-breaking due to the wealth and quality of clinical and bacteriological data to match with biomarker responses,” Hu said. “The new insights gained will promote future work in the field of markers of treatment response in children with TB. This research is critical to pave the way to more appropriate management of children with TB.”
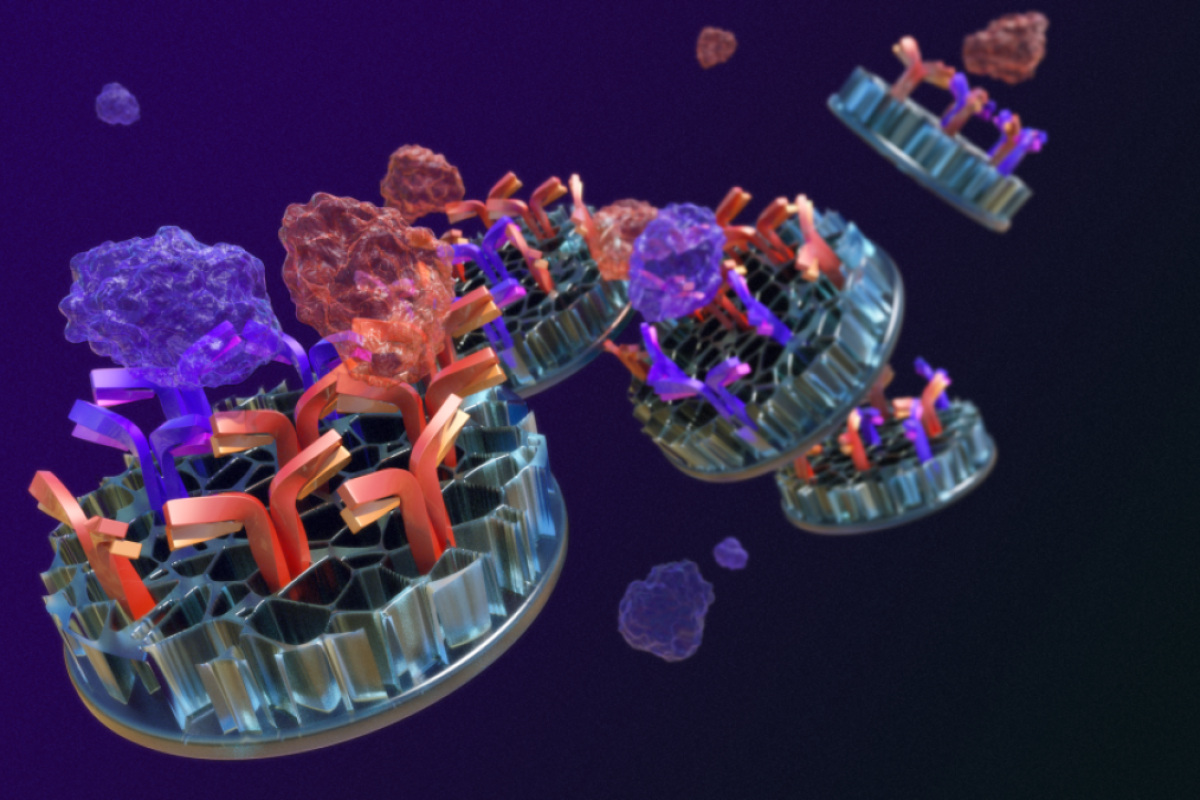
With the NICHD funding support, Hu’s team will combine the powers of advanced nano-sensing technology and TB molecular biology, and intend to optimize and validate a quantitative biomarker detection and monitoring platform that works in tandem with “miniaturized” mass spectrometry.
At the core of the technology, Hu’s lab developed nanoparticles with very specific antibodies attached, through which blood and eventually urine samples can be used to detect TB. This is a much faster and less invasive approach than the current methods of coughing up sputum, biopsy, spinal taps or growing blood cultures.
For this grant, Hu’s lab has partnered with Stellenbosch University's Desmond Tutu Tuberculosis Centre to test blood samples from infected patients. South Africa has the fourth highest TB rate in the world, while the Western Cape Province has the highest number of new TB cases in the country, the Desmond Tutu Centre is in the unique position to have access to a large variety of samples from their community.
The grant aims to validate and develop a quantitative model for active TB in which they could potentially test the effectiveness of treatment as well by testing the blood at various time intervals throughout treatment.
“The proposed work on evaluating our Nanoparticle-MS assay as a marker of TB treatment response will ensure unprecedented in-depth engagement with the bioanalytical and clinical data, and thus improve data management and interpretation of results, leading to clinically relevant outputs, and new hypotheses and insights,” Hu said.
Eventually, once the system has been refined the goal would be to us this accurate, high-throughput testing method with an easy-to-use shoe-boxed size detection system which would allow this technology to reach some of the world’s populations that are most in need.
Written by: Lerys del Moral, freelance science writer
Media contact: Joe Caspermeyer, Joseph.Caspermeyer@asu.edu
More Science and technology

Turning up the light: Plants, semiconductors and fuel production
What can plants and semiconductors teach us about fuel production?ASU's Gary Moore hopes to find out.With the aim of learning how…

ASU technical innovation enables more reliable and less expensive electricity
Growing demand for electricity is pushing the energy sector to innovate faster and deploy more resources to keep the lights on…

What do a spacecraft, a skeleton and an asteroid have in common? This ASU professor
NASA’s Lucy spacecraft will probe an asteroid as it flys by it on Sunday — one with a connection to the mission name.The asteroid…