Antimicrobial chemicals in indoor dust associated with higher count of antibiotic-resistance genes

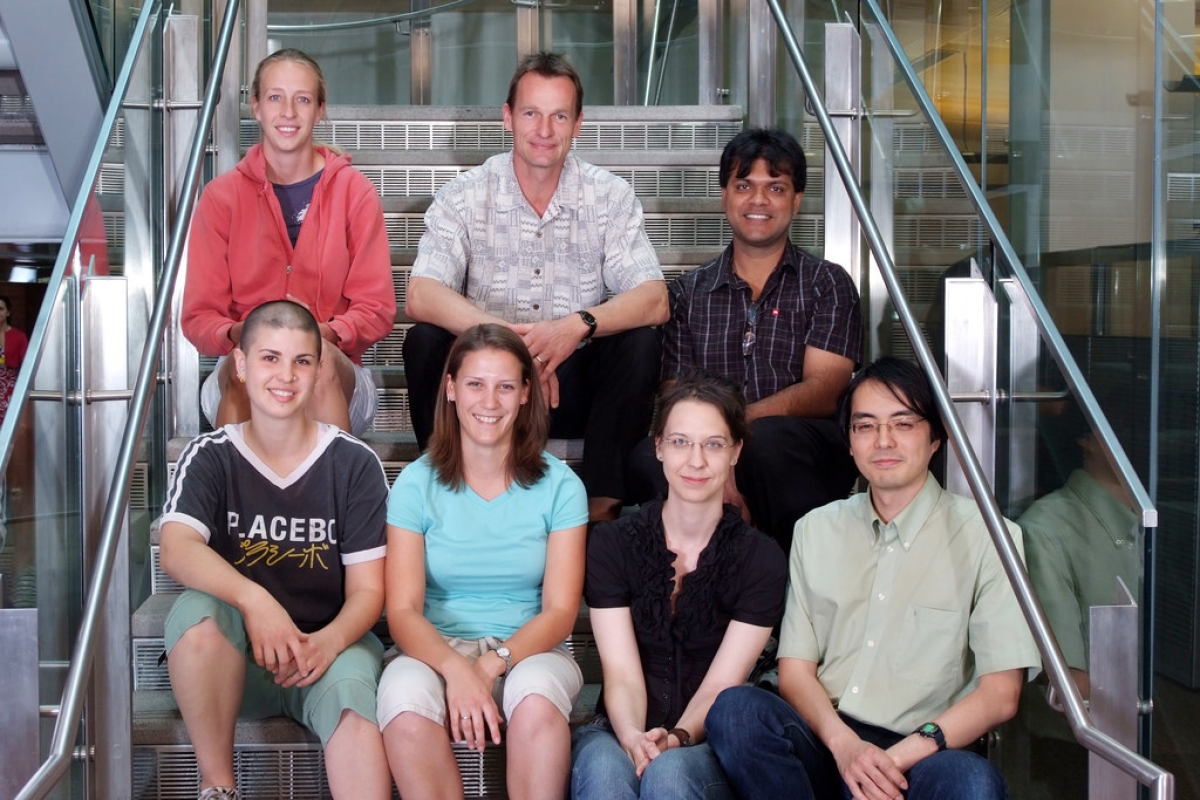
Researcher Erica Hartmann collects dust samples for her study, done in collaboration with Biodesign's Center for Environmental Security, led by Rolf Halden.
In a collaborative study involving four major universities, researchers have found links between the levels of antimicrobial chemicals and antibiotic-resistance genes in the dust of an aging building used for athletics and academics.
The association was particularly striking for triclosan, the most commonly used antibacterial ingredient in personal-care products. Whereas the study design investigated co-occurrence rather than causation, the study does point to a probable cause worthy of more exploration. In the laboratory, triclosan is known to foster in microorganisms the development of cross-resistance to clinically important antibiotics. Up until now, studies were lacking either demonstrating or suggesting that the selection for drug resistance also may have implications for public health in real-world settings.
"We might be tempted to think of the antimicrobial chemicals as being guilty by association," said Erica M. Hartmann, a postdoctoral fellow at the University of Oregon's Biology and the Built Environment Center and Institute of Ecology and Evolution who led the study. In September she joins the faculty at Northwestern University, after being a Fulbright Scholar and a former graduate student in Arizona State University professor Rolf Halden’s Biodesign Insitute research center.
"We don’t really know how the genes or the chemicals got there," she said. "They may have arrived by completely different routes and their being found together is a coincidence. However, we know that antimicrobial chemicals can cause an increase in antibiotic resistance in other situations, so I think these results provide a good reason to take a closer look at what’s going on in dust."
The study, published online ahead of print in the journal Environmental Science & Technology, is the first to document the coexistence of the chemicals and genes in indoor dust.
In all, the paper reports six significant associations. Levels of triclosan and other antimicrobials in dust were determined in collaboration with the Biodesign Center for Environmental Security at ASU and analyzed by doctoral research assistant Jing Chen. Center director Halden notes that “these new findings merit follow-up studies because house dust is inhalable and thus represents a potentially important pathway of exposure to antibiotic-resistance genes and drug-resistant bacteria.” He adds, “The efficacy of antimicrobial additives to soap has long been questioned; the new findings reported here provide one more reason to reassess both the need for and safety of triclosan."
On Sept. 2, the FDA agreed with Halden's assessment and scientific evidence, ruling to ban more than 19 ingredients, including the removal of triclosan and triclocarban from more than 2,000 over-the-counter antibacterial hand- and body-wash products. Manufacturers will have one year to comply with the rulemaking by removing products from the market or reformulating (removing antibacterial active ingredients) these products.
The antimicrobial chemical triclosan has been linked with a gene that alters the ribosome — a complex of RNA and protein in cells that is responsible for RNA translation — in a way that makes bacteria antibiotic-resistant. The research team identified several antibiotic-resistance genes, the most common of which conferred resistance to tetracycline antibiotics. "While present at low abundances, together these genes cover resistance to a wide spectrum of antibiotics," the researchers wrote.
The chemicals and genes came from 44 samples from 31 varied-use spaces, using vacuum-fitted collectors. The building, completed in 1921, has window ventilation as well as infiltration of outdoor air through cracks around doors and windows. DNA processing involved the UO Genomics Core Facility, and data were processed with assistance from the lab of co-author Curtis Huttenhower of Harvard University's School of Public Health.
Despite the findings, Hartmann said, people don't need to be readily alarmed. Antibiotic-resistance genes in the environment, for example, are 10 to 100 times less abundant than in the human gut, she said. In infants, the genes occur naturally in the absence of antibiotics during initial microbial colonization.
"Antibiotic resistance is common in a lot of different places," she said. "Just because we find it in a certain building doesn’t mean that everyone who goes into that building is going to get a MRSA infection. The building is still as safe as it was before the study, but now we have a better idea of how many antibiotic-resistance genes there are, and we have reason to believe that the amount of antibiotic-resistance genes may be tied to the amount of antimicrobial chemicals."
Associations of triclosan and antibiotic resistance have been found in other places and in the environment, Hartmann said, but finding the association in indoor dust brings the threat a lot closer to home. Median concentrations of triclosan found in the dust were much less than those found as the active ingredient in toothpaste. The chemical also is widely used in antibacterial soaps.
"The World Health Organization has said that we’re underestimating community-acquired antibiotic-resistant infections," she said. "We know that hospitals and other health-care settings are burdened by antibiotic-resistant pathogens. Homes and other buildings also can contain antibiotic-resistance genes, and and the use of antimicrobial chemicals in these buildings may be a contributing factor."
Co-authors included first author Erica Hartmann, Roxana Hickey, Clarisse M. Betancourt Roman, Jeff Kline, G.Z. Brown and Jessica L. Green from the University of Oregon; Curtis Huttenhower, Tiffany Hsu and Randall Schwager from Harvard T.H. Chan School of Public Health and Broad Institute of the Massachusetts Institute of Technology; and doctoral student Jing Chen and Rolf U. Halden from the Biodesign Center for Environmental Security at Arizona State University’s Biodesign Institute.
The Sloan Foundation, National Science Foundation and National Institutes of Health supported the research.
More Health and medicine

Bird flu: Your questions on symptoms, spread and safety answered
Bird flu is no longer only “for the birds.”Infections have expanded beyond wild birds and poultry to a range of animals — from…

Making medicine side-effect free
Many drugs that address medical conditions can come with serious side effects. In drug commercials, the litany of potential side…

Diagnostic research happening at ASU focused on detecting diseases earlier to save lives
It was one of America’s founding fathers, Benjamin Franklin, who may have foreshadowed today’s health care innovation when he…