Switched-on Salmonella

Non-Typhoidal Salmonella causes widespread illness in America and around the globe, producing symptoms of food borne illness, including gastroenteritis. A particular strain in sub-Saharan Africa known as ST313, however, is the cause of (often fatal) blood infections. Both types of Salmonella respond to fluid shear forces, though they do so in different ways, as the new study shows. Photo by: Jason Drees: Biodesign Institute
Once inside the human body, infectious microbes like Salmonella face a fluid situation. They live in a watery world, surrounded by liquid continually flowing over and abrading their cell surfaces — a property known as fluid shear.
In new research appearing in the Nature Publishing Group journal npj Microgravity, Cheryl Nickerson and her colleagues explore the effects of physiological fluid shear on ST313 — a particularly dangerous type of Salmonella, which is resistant to multiple antibiotics and currently ravaging regions of sub-Saharan Africa.
Unlike “classic” Salmonella strains that cause gastroenteritis, intestinal disease is often absent during ST313 infections and isolates are most commonly recovered from blood, rather than stool. Recent epidemic outbreaks of ST313 in sub-Saharan Africa highlight the pressing need for better mechanistic models of infection and disease progression.
The new study shows — for the first time — that fluid shear forces regulate disease progression not only in well-studied Salmonella stains causing gastroenteritis, but ST313 strains as well. Specifically, high fluid shear forces accelerated disease onset and enhanced the ability of Salmonella ST313 strain D23580 to survive stressful conditions encountered during infection.
Interestingly, the response of D23580 to fluid shear was different from that of “classic” Salmonella causing intestinal infections, suggesting that different fluid shear forces encountered by pathogens in the intestinal tract versus bloodstream can differentially impact disease progression.
The potential for the physical force of fluid shear to drive pathogen responses and infectious disease outcomes is a pioneering concept first proposed by the Nickerson team. Their discoveries have served as a foundation for the rapidly growing field of bacterial mechanotransduction (the ability of bacterial cells to sense and respond to physical forces) and how it relates to infectious disease.
“The results of this study shed new light on the physical force cues that may be used by ST313 strains during the natural course of infection to determine their location in the body and initiate disease specific programs,” Nickerson said. “This finding could reflect differences in evolutionary adaptations between Salmonella strains causing intestinal disease and those causing more severe bloodstream infections. These findings may lead to new targets for the development of urgently needed therapeutics against multidrug resistant bacteria."
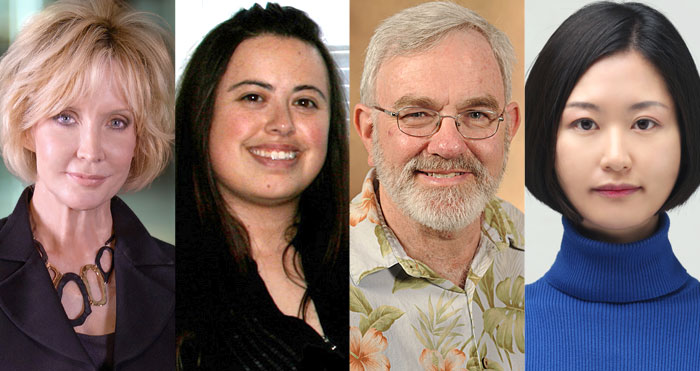
Biodesign Institute research team (from left): Cheryl Nickerson, Jennifer Barrila, Ken Roland and Jiseon Yang. Photo courtesy of Biodesign Institute
For this study, bacterial cells were cultured in a device known as a rotating wall vessel bioreactor (RWV). Originally developed by NASA, the RWV has been used to culture cells under fluid shear levels that simulate conditions found in the human body, as well as those encountered during spaceflight. Nickerson and her colleagues had previously demonstrated that RWV bioreactors provide a powerful platform for studying host-pathogen behavior.
Studies like the present one offer vital insights into the means by which ST313 and other invasive pathogens infect the body, colonize tissue, evade host defenses and cause illness.
Nickerson is interim co-director of the Biodesign Center for Infectious Diseases and Vaccinology at Arizona State University. For the new study, postdoctoral researcher Jiseon Yang and Assistant Research Professor Jennifer Barrila at the Biodesign Institute are co-lead authors. They are joined by associate research professor Kenneth Roland at Biodesign, and Mark Ott at the NASA Johnson Space Center. (Nickerson is also a professor in ASU’s School of Life Sciences.)
Many-faced threat
Pathogenic Salmonella bacteria fall into two broad categories: typhoidal and non-typhoidal (or NTS strains). The former — responsible for typhoid fever — include Salmonella Typhi and Paratyphi. Such pathogens are said to be “host-restricted,” targeting only humans and higher primates.
Typhoidal strains of Salmonella cause severe blood borne infections and are more common in underdeveloped countries, where contaminated water often harbors the bacteria. Left untreated, typhoid fever can lead to shock, organ failure and death.
Non-typhoidal forms on the other hand, are ubiquitous, causing one million foodborne illnesses annually in the United States alone, with 19,000 hospitalizations and 380 deaths, according to the Centers for Disease Control. Non-typhoidal Salmonella (NTS) strains are the leading cause of bacterial food-borne illness, which typically involves gastrointestinal distress, nausea, vomiting and diarrhea.
Over 2,500 variant forms of NTS exist. Unlike typhoidal strains, non-typhoidal Salmonella varieties are zoonotic—infecting a wide variety of animal hosts, including humans. Typically, non-typhoidal Salmonella bacteria are transmitted through the consumption of contaminated food, particularly meat, poultry, eggs and milk. While no vaccine exists for non-typhoidal Salmonella, associated illness is usually self-limiting in healthy people.
Emerging multidrug resistant strains menace Africa
While categorized as non-typhoidal pathovars, ST313 Salmonella strains appear to lie somewhere in between the conventional designations of typhoidal and non-typhoidal Salmonella. Often, afflicted individuals do not experience the gastrointestinal distress commonly associated with NTS infections. Rather, ST313 is a major cause of fatal blood infections in young children affected by malaria, severe anemia and/or malnutrition, as well as adults infected with the HIV virus.
Invasive non-typhoidal Salmonella, like ST313, are an important cause of illness in children under the age of five years in sub-Saharan Africa. These strains often display multi-drug resistance and cause septicemia, meningitis and other serious complications, and are often fatal.
Given the highly drug-resistant nature of ST313, effective treatment is challenging, particularly in resource-poor regions with inadequate health infrastructure. Fatality rates for children range from 20-25 percent, while rates for HIV-positive patients may run as high as 50 percent.
“This study indicates that physical force niches in the infected host may drive dynamic pathogen responses and adaptation which are important for disease progression,” said Yang. “Our findings may serve as a foundation for development of new strategies to effectively combat emerging and reemerging pathogens, which currently threaten the health of millions globally."
Shear magnitude
As the authors have repeatedly shown, bacterial responses to alterations in fluid shear are essential for regulating the infectious disease process in ways that often cannot be observed using traditional experimental approaches, in which bacterial cells are either shaken or held static in a laboratory flask. These traditional tests can fail to replicate the subtle mechanical cues vital to infection processes and disease development, thereby missing key parameters that are critical to understand how infectious disease happens in the human body.
Many factors contribute to a pathogen’s capacity to infect its host, including pH, temperature, oxygen, and nutrient availability. While ST313 has recently been shown to attack hosts of different species, albeit not as widely as NTS strains, the full range of potential hosts and animal reservoirs in sub-Saharan Africa is not known. The Nickerson team has previously shown that in addition to humans, mice can also be infected with ST313 strain D23580.
As Nickerson and her colleagues have previously demonstrated in a variety of earthbound and space-bound experiments, higher and lower levels of fluid shear forces flowing across bacterial cell surfaces can induce profound changes in the ability of “classic” gastroenteritis-inducing Salmonella to cause disease (virulence) and survive host defenses. However, the current work is the first study to look at the fluid shear response of any strain belonging to the deadly ST313 lineage, and showed that D23580 behaves very differently than classic NTS in response to these dynamic culture conditions.
When the researchers subjected ST313 strain D23580 to the fluid shear conditions of the RWV, the results were surprising. Unlike “classic” NTS strains, ST313 responded to physiological fluid shear conditions in an opposite manner, with virulence traits and stress defenses ramped up under higher fluid shear conditions. Specifically, a shorter time-to-death was observed for mice infected with D23580 cultured under higher fluid shear conditions.
The D23580 strain also exhibited increased resistance to low pH, bile salts, oxidative and osmotic stress conditions, which are natural antimicrobial defenses in the human body. Ongoing studies by Nickerson and her colleagues is aimed at clarifying distinctive disease mechanisms at work in this highly lethal pathogen.
“Historically, the importance of fluid shear in regulating disease-causing properties of bacteria was largely underappreciated. This study leverages from our previous findings indicating that bacteria are hardwired to respond to a variety of physical forces, including fluid shear. However, our current study shows these responses can differ even between closely related bacteria,” Barrila said. “Our future studies can perform additional comparisons with closely related strains to better understand specific mechanisms used by bacteria to sense and respond to fluid shear, differentially impacting their disease-causing properties.”
More Science and technology

Cracking the code of online computer science clubs
Experts believe that involvement in college clubs and organizations increases student retention and helps learners build valuable…
Consortium for Science, Policy & Outcomes celebrates 25 years
For Arizona State University's Consortium for Science, Policy & Outcomes (CSPO), recognizing the past is just as important as…

Hacking satellites to fix our oceans and shoot for the stars
By Preesha KumarFrom memory foam mattresses to the camera and GPS navigation on our phones, technology that was developed for…