ASU expert sheds light on the Zika virus
Molecular biologist talks about what we know about the virus — discovered in 1947 — and what we don't as outbreak continues

The Zika virus has brought us endless footage of masked men spraying insecticide in Brazilian slums and reports of babies with tiny heads — a rare condition called microcephaly — along with dire intonations.
World Health Organization officials have estimated that 1 million people are already infected in South America, and 4 million to 5 million more could be infected in 2016, as temperatures warm in the Northern Hemisphere.
ASU Now sat down with Arizona State University’s Brenda Hogue — a molecular biologist (pictured above) who studies how viruses replicate and assemble and how they impact host cells, ultimately contributing to disease — to spread some light on the topic.
This week HogueHogue is an associate professor in the School of Life Sciences, which is part of the College of Liberal Arts and Sciences. will take part in a public lecture and panel discussion called “Zika Virus: Understanding the Outbreak” with other experts from ASU and public health officials. The public event is aimed at providing current and accurate information regarding the Zika virus outbreak. It will be held from 7-8:30 p.m. Thursday, Feb. 25, on the Tempe campus. Find more event details here.
Question: This was discovered in Uganda in 1947. Why is it jumping out at us now?
Answer: It was initially discovered in 1947 during surveillance for yellow fever. It was isolated from a monkey. The virus has been sporadically occurring there in that area. It really didn’t seem to cause significant problems for people. Also, there’s a complication that we really don’t have any good diagnostics for it. At that time it was like OK, it’s one of these viruses like yellow fever. Because there didn’t seem to be any major outcome — individuals recover — they found it mostly in mosquitoes and in some of the primates there. There is a complication with the diagnostics. You can be misled because there is cross-reactivity with dengue and with some of the other viruses that are mosquito-borne.
Q: So it can be mistaken for something else?
A: That’s right. There may have been more cases in the time since it was discovered, but we just weren’t aware of it. Of course then it moved over into other areas like the French Polynesian islands. Again, there, while there were these outbreaks, it wasn’t really considered to be that serious. It’s in an area where you have dengue and chikungunya. It’s now really acutely come to our attention because of the rapid spread as it’s moved through the Western Hemisphere.
Q: Is that why it’s in the news? Is that why it has caught our attention?
A: Yes, the virus wasn’t initially in the Western Hemisphere. It was in Africa initially and then it moved into some Asian areas. … When it moved into Brazil, where it was first detected in the Western Hemisphere, it has just very rapidly — within a year — moved all through Brazil and though the northern part of South America and over into Mexico and some areas of the Caribbean.
Q: How worried should people be about it?
A: It is like many of these viruses that are spread by a vector like mosquitoes. Some of the viruses, like dengue and chikungunya, are more serious in terms of some of the potential that they have for the disease they cause. All of these, many individuals will be infected, including Zika, individuals who are healthy and may never realize they were infected with the virus.
Q: Kind of like Valley fever — they get it and never know they had it.
A: And then at some point they’re checked: “Oh, you must have had it.” In terms of the concern, the symptoms are like the common cold, maybe some fever. For the Zika, some individuals have a light rash but not anything that would be of such significance that you would probably pay very much attention to it. Some weakness — the typical things that you have with influenza. Then there have been reports of cases where there has been a suggested correlation with microcephaly. There have also been some neurological conditions like Guillain–Barré syndromeGuillain–Barré syndrome is an autoimmune disease in which the body’s immune system attacks the nerves, causing rapid-onset muscle weakness and sometimes paralysis. In rare cases, it is life-threatening when the breathing muscles are affected.. Those are rare, but there is this correlation that has been suggested between the microcephaly and infection during pregnancy.
Q: Has that been proven?
A: That has not been proven. There’s a lot of work that needs to be done in that area, and there is a lot of work that is starting to be done. That is one of the biggest concerns for pregnant women. It is a concern for us here in the U.S., but it’s not something we should be in a panic about. I think it’s like West Nile. It’s easy to see it moving across the U.S. Again, you can have a very low percentage of people who do develop neurological conditions, and some people do die, mostly the elderly. For the most part, people don’t know they’ve been infected or they will have very mild symptoms.
Q: So this is not something we should run screaming to the hills about?
A: No. I think that the concern is that because it hasn’t come into this country other than with people who have traveled to that area, is that the mosquitoes who transmit the viruses will move up. We have those mosquitoes here. It’s just that they are not carrying the virus yet.
We have the Aedes aegyptiThe Aedes aegypti mosquito is the main vector that transmits the viruses that cause dengue and, it is believed, Zika. here in Maricopa County. It moved in a few years ago. It likes urban areas, areas where you have moisture and a little bit of standing water. It’s very prevalent in the Southeast. One of the concerns is that one of the mosquitoes that transmits this will move up here.
The Aedes aegypti mosquito is drawn to urban areas where there is a bit of standing water. Photo by U.S. Department of Agriculture via Wikimedia Commons
One of the biggest and best preventions is to carry out mosquito control. In this country there are certainly some areas — lower-income areas, usually — where there might not be as good a protection, but generally in this country we use air-conditioning, have screens on our windows, we do mosquito control when necessary. That helps tremendously. That’s our major line of defense. But at this point it has not come. Mosquitoes that are carrying it have not come. There are two ways mosquitoes could come: They could cross the border easily or people who have been to those areas could carry it.
Q: So there are still a lot of unknowns.
A: There are a lot of unknowns at this point.
Top photo: Brenda Hogue in her Tempe office. Photo by Deanna Dent/ASU Now
More Health and medicine
ASU center hosts community gathering to discuss latest health research
Communication and collaboration were front and center as Arizona State University’s Center for Health Information and Research, or CHiR, met with community partners and other stakeholders on April 3…
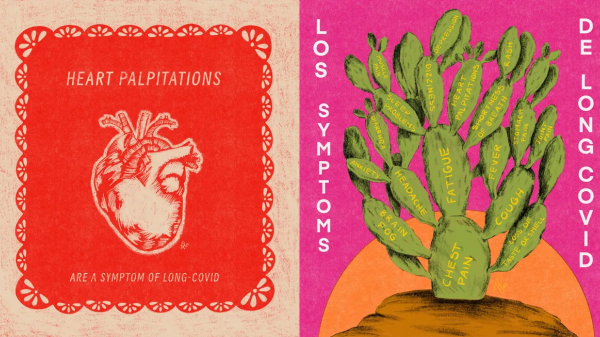
Health communication program brings long COVID awareness to Latinos
After COVID-19 hit the Latino community especially hard, Gilberto Lopez created COVIDLatino, a health communication program designed to share accurate, timely, evidence-based and culturally tailored…
Gates Foundation to fund research on antibiotic resistance
Antibiotic resistance, what happens when germs develop the ability to defeat the drugs designed to kill them, is a growing concern among scientists today. When bacteria become resistant to…
