ASU researchers working to develop biomarkers to screen for HPV-related cancer
Graphic by Jason Drees.
Recent studies have highlighted a concerning trend: a rise in oropharyngeal cancer — difficult to diagnose and difficult to treat — linked to the human papillomavirus (HPV).
Researchers are keen to spread awareness about this connection, emphasizing the importance of HPV vaccinations for both men and women and expanded testing for those at risk.
In new research, Dr. Karen Anderson and her colleagues explore sophisticated new methods for screening for this form of cancer, which has previously evaded early detection.
A new, $4.8 million five-year grant from the National Cancer Institute and National Institutes of Health will help researchers develop cancer biomarkers — telltale indicators of disease — that can be detected in saliva and blood samples by using microarray and PCR technology.
Currently, there is no screening program for oropharyngeal cancer, making early, life-saving diagnoses particularly challenging.
“This is a great opportunity to combine the expertise in molecular diagnostics at ASU with colleagues across the country to develop cancer screening for head and neck cancer,” says Anderson, principal investigator of the new grant.
Anderson is a researcher in the Biodesign Virginia G. Piper Center for Personalized Diagnostics and a professor with the School of Life Sciences at Arizona State University.
The goal of the new study is to evaluate screening strategies and biomarkers for the early detection of HPV-associated head and neck cancers, with an emphasis on the use of saliva for rapid screening. Anderson is joined by ASU Biodesign Institute researcher Vel Murugan.
Research collaborators include Ann Spolarich with the AT Still School of Dentistry; Drs. Erich Surgis and Kristina Dahlstrom with Baylor College of Medicine, Houston; and Meso Scale Diagnostics, LLC, Rockville, Maryland.
The research will be conducted under the auspices of the Southwest Clinical Validation Center for Head and Neck Cancer. The group is one component of an ambitious, multi-institute consortium organized by the National Institutes of Health and National Cancer Institute, known as the Early Detection Research Network.
HPV: A silent prelude to cancer
HPV is the most common sexually transmitted infection in the United States. The Centers for Disease Control and Prevention has estimated that nearly 80 million Americans are currently infected with HPV, with approximately 14 million people becoming newly infected each year.
HPV is a group of more than 200 related viruses. Some, if left untreated, can lead to cancer. Until recently, HPV was mainly linked to cervical cancer in women. But more recent studies show that certain high-risk HPV types are becoming a significant risk factor for oropharyngeal cancer.
Further, the demographic of patients afflicted with oropharyngeal cancer appears to be changing. Many are now younger, with no history of tobacco or alcohol use, prompting an increased focus on HPV as a potential causative agent.
Oral HPV is transmitted to the mouth by oral sex, and possibly in other ways. About 10% of men and 3.6% of women have oral HPV, and oral HPV infection is more common with older age. While most will clear HPV within one to two years, HPV infection can also persist in some people.
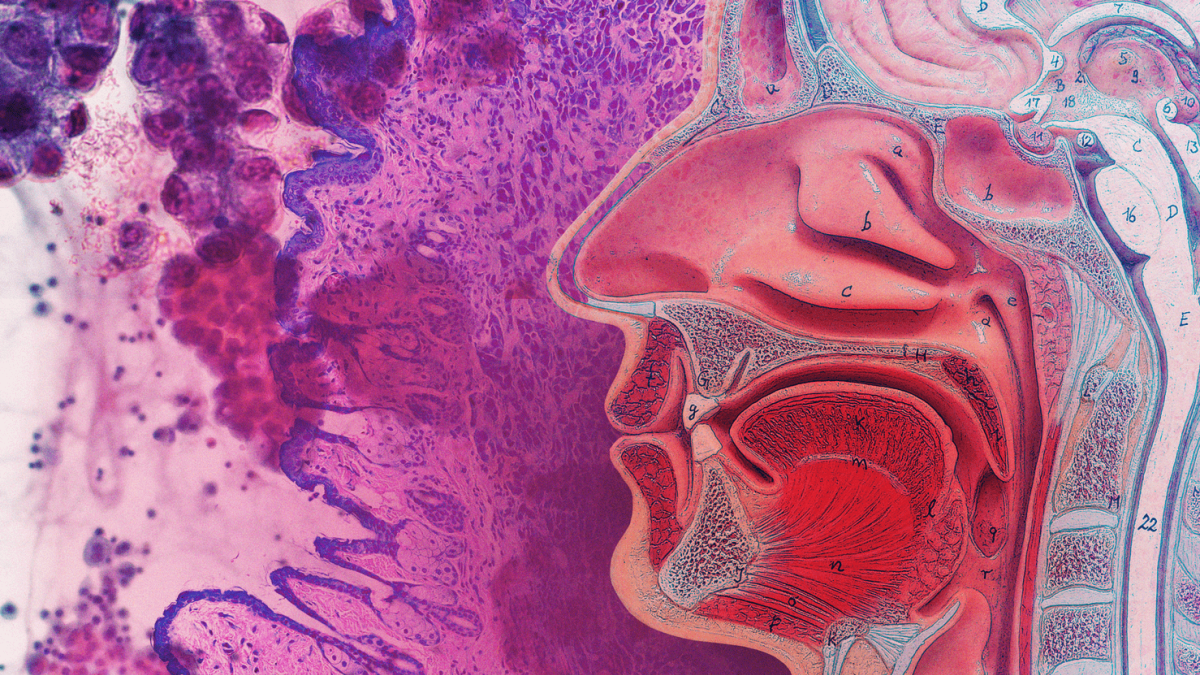
The HPV virus can infect the mouth and throat and cause cancers of the oropharynx (back of the throat, including the base of the tongue and tonsils), a condition known as oropharyngeal cancer. HPV is thought to cause 70% of oropharyngeal cancers in the United States.
Historically, tobacco and alcohol use have been major risk factors for this aggressive form of cancer. However, researchers are now shedding light on a different potential cause — HPV.
The slow transition from infection to cancer
Usually, it takes years after being infected with HPV for cancer to develop. It is unclear if having HPV alone is enough to cause oropharyngeal cancers or if other factors (such as smoking or chewing tobacco) interact with HPV to cause these cancers.
Symptoms of oropharyngeal cancer may include a long-lasting sore throat, earaches, hoarseness, swollen lymph nodes, pain when swallowing and unexplained weight loss, though many cases produce no perceptible symptoms.
The HPV vaccine was developed to prevent cervical and other cancers of the reproductive system. The vaccine also protects against the types of HPV that can cause oropharyngeal cancers. The CDC recommends HPV vaccination for 11- to 12-year-olds.
Vaccination for everyone through age 26 years is also recommended, if not vaccinated already, however vaccination for those older than age 26 years provides less benefit, as more people have already been exposed to HPV. HPV vaccination prevents new infections but does not treat existing infections or diseases. This is why the HPV vaccine works best when given before any exposure to HPV.
In addition to vaccination, early detection of oropharyngeal cancer also remains critical. Regular dental checkups can often detect early signs of oropharyngeal cancer, dramatically improving the chances of successful treatment.
“In cancer, screening and early detection can prevent the disease from progressing, reduce the risk of complications and improve long-term health,” Murugan says. “Our goal is to develop and validate an easy-to-use, cost effective, non-invasive diagnostic test to screen a large segment the population and inform anyone who is susceptible to this terrible disease. We will build upon the sizeable amount of data generated by Dr. Anderson and her group to accomplish this, using saliva as a biospecimen.”
Developing effective biomarker tests
A biomarker is a measurable indicator of some biological state or condition. It could be a molecule secreted by a tumor or a specific response of the body to the presence of cancer. Biomarkers can be used for various purposes, including disease diagnosis, prognosis, prediction of treatment response and monitoring of disease progression.
Despite many years of research, there are very few biomarkers for oropharyngeal cancer that have been validated in a laboratory setting that comply with the Clinical Laboratory Improvement Amendments (CLIA) and College of American Pathologists standards.
The new research hinges on a comprehensive understanding of the carcinogenic progression induced by HPV in the oropharynx over decades, yielding distinct circulating and salivary viral nucleic acid and blood-borne markers.
Previous research by the group demonstrated that the presence of HPV can be reliably predicted using an array containing a combination of different antibodies specific to a particular form of HPV. The strategy is known as a multiplexed panel.
Given the low incidence of this form of cancer in the general population, the center will apply innovative strategies of self-collection sampling, digital enrollment and distributive systems, enhancing accessibility and inclusivity, particularly in underserved communities.
More Science and technology
From food crops to cancer clinics: Lessons in extermination resistance
Just as crop-devouring insects evolve to resist pesticides, cancer cells can increase their lethality by developing resistance to treatment. In fact, most deaths from cancer are caused by the…

ASU professor wins NIH Director’s New Innovator Award for research linking gene function to brain structure
Life experiences alter us in many ways, including how we act and our mental and physical health. What we go through can even change how our genes work, how the instructions coded into our DNA are…

ASU postdoctoral researcher leads initiative to support graduate student mental health
Olivia Davis had firsthand experience with anxiety and OCD before she entered grad school. Then, during the pandemic and as a result of the growing pressures of the graduate school environment, she…