TGen, ASU, Phoenix Children's collaborate to better treat fatty liver disease in Latino youth
The prevalence of nonalcoholic fatty liver disease, or NAFLD, is rising in American children, with kids of Latino ancestry being hit disproportionately hard by the disease.
This chronic condition can progress to more severe forms of liver disease, but experts are not yet able to determine which children are at greatest risk of progression. There are currently no approved treatments for NAFLD in children, apart from modifications in diet and physical activity.
In order to better understand this disease, researchers from the Translational Genomics Research Institute (TGen), part of City of Hope, and Arizona State University's Edson College of Nursing and Health Innovation have partnered with clinicians from Phoenix Children’s and Cincinnati Children’s on a new study.
Professor Johanna DiStefano, head of TGen’s Metabolic and Fibrotic Disease Program and a lead investigator on the project, will be using advanced molecular techniques to identify signatures of fatty liver disease in children. DiStefano has been investigating NAFLD for over 15 years.
“Pediatric NAFLD is associated with poor long-term outcomes, such as diabetes, cardiovascular disease and even increased liver-related mortality in adulthood. How exactly this happens — what cellular and molecular mechanisms contribute to this metabolic dysfunction and what roles are played by diet, lifestyle and environment — are still poorly understood,” DiStefano said, adding, “NAFLD is typically a silent disease and is often not discovered until it has reached advanced stages; therefore, there is a real need for this kind of work.”
This study was made possible through a five-year R01 grant of $3.9 million from the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health.
Specifically, the study will examine and characterize the cargo of circulating extracellular vesicles in NAFLD and determine what factors are different in kids with NAFLD compared to those without. Extracellular vesicles are known to exert influence over cellular signaling, wound repair and tissue remodeling in the liver.
“This study will give us a better idea why some kids get liver disease and others don’t," said Professor Gabriel Shaibi, director of ASU's Center for Health Promotion and Disease Prevention and co-principal investigator for the study. "We will also explore how changes in liver fat storage after clinical intervention may alter molecular markers of the disease. In the future, these findings could help doctors to develop better methods to diagnose and treat fatty liver disease in kids.”
Preliminary data forming the foundation for this study revealed protein signatures in extracellular vesicles that appeared specific to fatty liver; and following a lifestyle intervention, these signatures began to resemble those observed in children without fatty liver disease.
Each member of the multidisciplinary team will have a distinct role in the study.
ASU will provide samples and data from Latino youth with obesity and mild liver disease before and after intervention. Phoenix Children’s will provide samples and data from Latino youth with advanced liver disease, while Cincinnati Children’s will provide samples and data from Caucasian and African American youth with advanced liver disease who underwent bariatric surgery and whose liver disease was subsequently resolved. TGen will perform all of the molecular, proteomic and statistical analyses on those samples, converting them from raw data to actionable information and investigating the mechanisms by which these NAFLD-associated factors contribute to the development and progression of disease.
“We are seeing a high number of pediatric patients at risk for NAFLD, and this study will help us better understand the underlying mechanisms involved in NAFLD, which will lead to improvements in our ability to diagnose and treat the disorder,” said Dr. Micah Olson, pediatric endocrinologist at Phoenix Children’s.
The team hopes that their study will shed fresh light on the disease processes that make NAFLD so dangerous in children and identify improved methods for detecting the disease in earlier stages.
This story was written in collaboration with TGen.
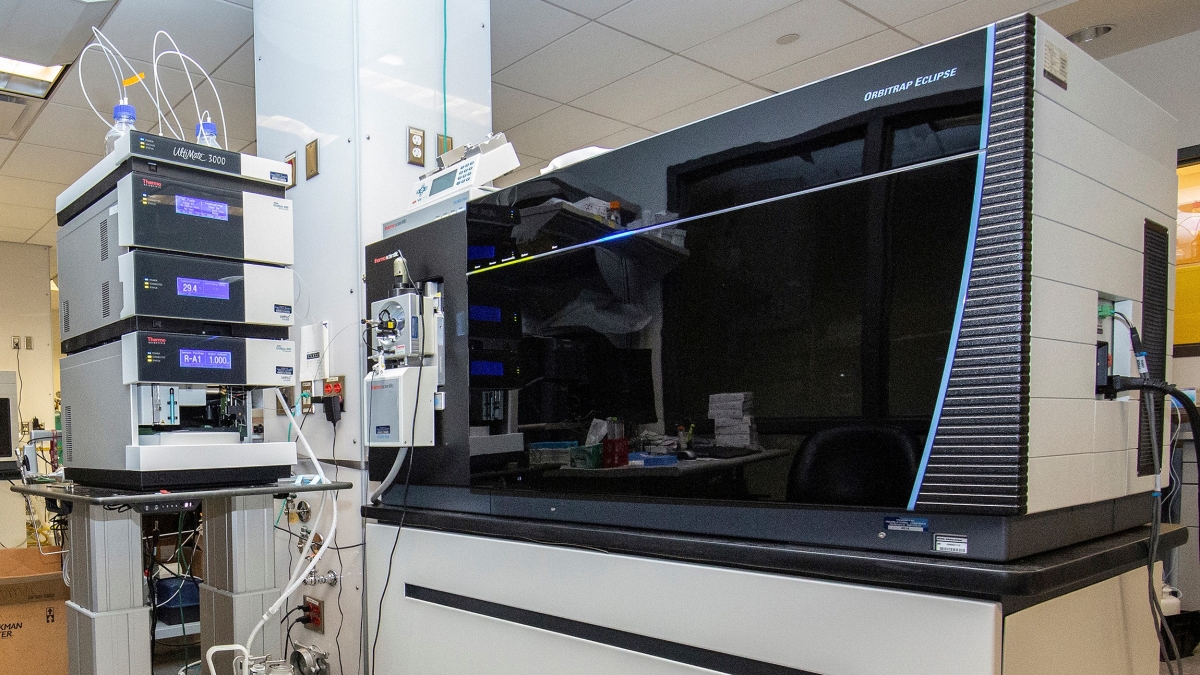
Top photo: Close-up of the Orbitrap Eclipse mass spectrometer that researchers at TGen will use this for the study. The machine examines protein structures to determine which proteins are in a compound. Photo courtesy Jeffrey Watkins/TGen
More Health and medicine
The surprising role of gut infection in Alzheimer’s disease
Arizona State University and Banner Alzheimer’s Institute researchers, along with their collaborators, have discovered a surprising link between a chronic gut infection caused by a common virus and…

ASU, University of Wisconsin partner to empower Black people to quit smoking
Arizona State University faculty at the College of Health Solutions are teaming up with the University of Wisconsin to determine which treatments work best to empower Black people to quit…

New book highlights physician wellness, burnout solutions
Health care professionals dedicate their lives to helping others, but the personal toll of their work often remains hidden.A new book, "Physician Wellness and Resilience: Narrative Prompts to Address…